Abstract
The thesis study aims at demonstrating that a career community pharmacist can practice as an effective clinician in a prescribing role treating patients in a primary care setting. The introduction of advanced and enhanced community pharmacy services enhances the need for pharmacists to integrate into primary care medical services. Non-medical prescribing, through the training with and subsequent prescribing within primary care, can incorporate community pharmacy into the primary care team if a satisfactory level of practice can be demonstrated. Treatment outcomes and standards of patient satisfaction with a pharmacist-led clinic were compared with the normal care of patients with hypertension at a Medical Centre. Pharmacist non-medical prescribing forms the core of the study and the historical devolution of prescribing rights will be considered as there are several levels of autonomy and range of medications that are available.
Introduction: Evolution of the Pharmacists in an Independent Prescribing Role
The pharmacy profession has developed from the earliest knowledge of herbal or mineral preparations that we’re able to offer the possibility of improving the health of a patient. The early pharmacist’s role, as it is understood today, was to prepare the medication in a form that made it possible for the patient to use these early drugs. Pharmacy practice required the combination of physical chemistry and botanical knowledge with the emerging medical health sciences to produce useful and probably effective drugs. There are many elements to the development of professional status for an occupation. For pharmacy, there is a specialized knowledge necessary initially, the ability to compound medicines that were required in order to be able to perform the role. Professional bodies, such as the Royal Pharmaceutical Society of Great Britain, were established to control entry into a pharmacy and ensure standards of education and practice were maintained.
As knowledge of drugs increased in the 20th century, a significant proportion of the traditional medicines were found to be either ineffective or potentially dangerous. Drug research and testing allowed pharmaceutical manufacturers to discover or design more effective medicines, which due to their potency required accurate control of the dose taken by patients. This led to one of the major features of medicine developed in the 20th century, the mass production of drugs into single-dose preparations such as tablets and capsules. At the start of the 20th century, pharmacy supply of medication usually required the physical preparation of an individualized medication according to a recipe ordered by a doctor for a specific patient. By the end of the century, most medication supplied from community pharmacies was in the form of mass-produced tablets and capsules.
The modern pharmacy profession has grown out of the supply of medicinal products to a population that could not afford the services of the early doctors. These medicines required preparation by mixing active, probably poisonous, ingredients with a variety of additional substances to produce an acceptable commercial product. These early medicines were then recommended for the treatment of specific ailments by the pharmacist and if successful, could lead to an increased reputation for the pharmacist or his ‘patent’ medication. The pharmacy profession has changed dramatically since the early 1800s when some chemists and druggists began to work together to promote the pharmacy profession. By 1841, this led to the formation of the Pharmaceutical Society of Great Britain by the leading pharmacists in London. Legal changes recognized the role of the Pharmaceutical Society to set professional examinations and register pharmacists under the Pharmacy Act 1852, without defining the professional role. Subsequent legislation in 1868 effectively gave pharmacists the right to sell, compound and dispense poisons with the Pharmaceutical Society being given the role of prosecuting pharmacists in cases relating to poisons. The preparation of safe stable medicines by the compounding of potentially poisonous chemicals and plant products was a key component of early pharmacy practice.
The professional practice of pharmacy has changed considerably over the past 40 years across all sectors. Most of the pharmacists in the United Kingdom practice in the community or retail sector, supplying medication to the public through over-the-counter (OTC) sales or by supply in response to a prescription from a medical or dental prescriber. In the UK there has been a division of the prescribing of medicines, largely under the control of the medical profession and dispensing normally by pharmacists but in some rural situations by dispensing doctors. In 1968 the legal classification of medicines was introduced with the safest medicines being labeled as general sales list, ‘GSL’ available to be sold by anyone, ‘P’ medicines which were only to be sold in pharmacies or prescription-only medicines, and ‘POM’s, which could not be obtained without a doctor’s prescription.
While there has been a steady process of change in the retail aspects of community pharmacy, the changes in dispensing economics have been achieved quite infrequently by changes to the NHS dispensing contract. In 1978, the rate of change in business organizations was expected to be a minor change each year and a major change every four to five years. Most probably, for most business sectors the rate of change has markedly increased over the last 30 years. In contrast, the changes to the dispensing contract have in the past occurred only once in a generation.
Present Scenario
At present, it is apparent that the development of manufactured medicines does not require a pharmacist to practice the medication compounding skills that were crucial to a pharmacist one hundred years ago. Pharmacists have found it almost compulsory to attain new skills to allow it to retain its professional integrity as it moves into the 21st century. The basis of professional status and how the profession of pharmacy has transformed from product-focused physical chemistry expertise to a patient-centered clinical role is the central view of this section. General dissatisfaction with the levels of professional practice in pharmacy, arising from a reduction in the exercise of medication compounding skills, led to an intellectual debate in the late 1970s and 1980s. It was then claimed by some academics that pharmacy might have lost the right to claim professional status. In the USA, Hepler and Strand believed that the reduction in the use of dispensing skills undermined the right to professional recognition. (Hepler C D and Strand L M 1990).
Pharmaceutical care in USA
‘Pharmaceutical Care’ was introduced in the USA hospital pharmacy sector and was defined as “the care that a given patient requires and receives which assures safe and rational drug usage” (Mikeal et al. 1975). This led to pharmacists being given patient counseling roles on hospital wards to enhance concordance with the medication at the hospitals. Advice on how to respond to the potential adverse effects of medication and thus decrease avoidable hospital admissions was an early focus of this clinical role. This role was further extended into a ward pharmacy role where pharmacists began to give advice on the choice of medication as it was prescribed to reduce the number of prescriptions for preventable adverse drug reactions with a significant decrease in the rate of adverse drug effects.
While the clinical roles were being introduced in hospital pharmacies, there was not much change in the community pharmacy sector. The community pharmacies, in the latter part of the 20th century, continued to perform the medication supply role for most United Kingdom citizens whether providing medication in accordance with a prescription, National Health Service or from a private doctor, or by over-the-counter sales. As the National Health Service pharmacy contract did not provide for any non-medication supply roles for community pharmacists, it might not be surprising that for many years little progress was made towards developing new community clinical roles.
There are several reasons for the lack of willingness to accept the new clinical practices seen in hospital pharmacy practice by the community pharmacy sector. Some of the major factors that hindered change were the lack of financial incentive, the lack of a unified profession, and low levels of participation in professional education after qualification as a pharmacist.
Pharmacy Contract with National Health Service
The community pharmacy contract with the National Health Service was initially based on the assumption that community pharmacy in the UK was a mixed role business. The pharmacies often developed a significant proportion of their income from commercial activity, such as by selling over-the-counter medicines, toiletries, photographic goods and baby care products. On account of this commercial activity, the National Health Contract initially paid pharmacist contractors a small fee for dispensing a prescription item and an element of profit, or on cost percentage, with additional fees for actually compounding prescription medication. While some pharmacists adopted a more clinical approach to professional practice, there was no clause in the National Health Service contract to reward this. The community pharmacists in the 1960s and 1970s mostly used to work as sole proprietors of independent businesses with little contact with their professional peers. The local pharmacists were normally viewed as business rivals and this did little to encourage a unified approach by the profession for developing new roles. It is probable that the failure of the Nuffield Inquiry to result in any significant change in the practice of pharmacy was on account of the lack of a unified professional voice calling for professional development. It will be observed afterward that the creation of a pro-change attitude within the community pharmacy sector was crucial to the agreement of the new pharmacy contract. At the same time, the need for continuing professional education was being reviewed. An inquiry commissioned by the government led to the adoption of an understanding that pharmacists and their staff should be required to keep their professional knowledge up to date with the latest developments and scientific know-how. Previously, post-graduate education was not compulsory for the profession and most pharmacists could either pick up what education they felt they needed from the Pharmaceutical Journal or allow their knowledge to be based on their pre-qualification university education.
In order to allow the community pharmacy to move away from the image of being shopkeepers, the on-cost or profit element of the medication dispensing process was removed. Instead, the pharmacists were paid a dispensing fee and a practice allowance which duly recognized the role the pharmacists played in public health education and medicines advice linked with over-the-counter sales. It had been proposed that amendments would be made to the supervision of pharmacies which would have allowed the pharmacists to delegate the dispensing process to their staff but this proposal was rejected by the profession. In the absence of an agreement on changing the supervisory rules which required the presence of a pharmacist in the pharmacy at all times, it was impossible to introduce new professional roles. It was to be a generation before the next major change which happened in community pharmacy arrangements with the National Health Service. The community pharmacists in an independent prescribing role in the General Practitioner practice, therefore assume greater significance. The broad knowledge base of medicines of the pharmacists also enables them to support patients with complex therapeutic regimes. Using the pharmacist prescribers has helped to improve the patients’ knowledge and compliance, which should lead to improved outcomes.
National Initiatives in Healthcare
With a number of national initiatives in healthcare being developed in the UK, added to those that are already part of routine care, there will be a significant impact on the way healthcare is delivered in the primary care setting. Some of these initiatives include Our Health, Our Care, Our Say and the Care Closer to home agenda, thus increasing the number of clinical domains in the new general Medical services Quality and outcomes Framework (QoF), and the commitment to increase primary care access for patients at evenings and weekends. Non-medical prescribing is thus an excellent way to maximize the skills of the existing staff in the National Health Service (NHS) to support the delivery of the NHS agenda and initiatives in the country.
Models of pharmacist prescribing in UK
Health Demographics of UK Population
At present, around 12% of the population in the UK, with some variance amongst regions and ethnicity, has hypertension, thus making it one of the largest treatable medical problems seen within primary care. Poor control of hypertension leads to several ailments such as stroke, diabetic complications and heart attacks. “…having high blood pressure is an important risk factor for developing stroke or heart attack in later life” (Bpassoc 2009). The increasing workload in the Healthcare segment due to demographic changes and lower treatment thresholds mean that the use of clinicians other than General Practitioners (GPs) for its management will be essential.
The hospital pharmacists, working at the National Health Service (NHS) in the UK, are ideally placed to be prescribers in a wide variety of clinical specialties. The hospital pharmacists have both a broad knowledge of medicines and a depth of specialist knowledge that has been gained through experience and postgraduate qualification. The medical records can be easily accessed, and they are able to monitor closely, the progress with therapy, and with the support of other clinicians including consultants. The specialist pharmacist roles allow the outpatient appointments and clinics to be managed by non-medical staff, with ready access to medical staff if necessary, which increases the clinical skills of specialist pharmacists, thereby improving team working and increasing access for patients.
Role of independent prescribing pharmacists in the care homes
The role of independent prescribing pharmacists in the care homes also assumes great significance. The National Service Framework for Older People describes how older people are most at risk of long-term conditions, non-elective hospitalization, falls, and other adverse events associated with medicines. At present, there are around half a million older people living in care homes in the UK, and they receive up to four times as many prescription items as those living in their own homes. The service users in the care homes are considered to be well provided for in terms of social and physical needs but it is also important not to overlook the need for person-centered healthcare. The role of pharmacists in Nurse independent prescribing in a walk-in center and out-of-hours care is also quite significant. At present, there are just over 90 walk-in centers across the United Kingdom that open for at least 15 hours a day, 365 days a year. The Walk-in centers are led by nurses and they generally deal with minor injuries (for example sprains, cuts) and minor ailments (for example allergies, pain, rashes).
The out-of-hours services are commissioned to provide urgent care outside core surgery hours. Under the new General Medical Services contract, the General Practitioners (GPs) are not required to provide 24-hour care for patients, so alternative providers operate a variety of services to allow patients to get medical advice and care at all times. The out-of-hours services are commissioned by the government to provide unscheduled care to patients outside core surgery hours, thus enabling the patients with access to medical care and advice at all times. The success and the expansion of the prescribing team are mainly due to the support of the medical director, lead nurse and the GPs who make up the out-of-hours team of clinicians. The primary care trust’s non-medical prescribing lead also supports the students by coordinating places on the course, placements and continuing professional development to ensure that all non-medical prescribers are able to keep up to date with therapeutic developments. Traditionally, the walk-in centers used a range of Patient group Directions to supply medicines, which could be time-consuming in terms of management and stock control. Having nurse independent prescribers at the out-of-hours centers means more patients have their episode of care completed by a nurse, and nurses can treat patients from outside the area who need prompt access to repeat medication. This flexibility is even more beneficial in the out-of-hours setting, where patient needs are often more wide-ranging.
Several General Practitioners (GPs), a pharmacist and a nurse have worked together to produce Clinical Management Plans for the patients. The Clinical Management Plans provide a framework in which to carry out medicine reviews, and the authority to make changes to medicines where necessary. The collaboration of three different healthcare professionals producing the Clinical Management Plans gives added value, with each person sharing and supporting the knowledge and expertise of the other. The only key challenge faced was acceptance by care home staff, although once relationships were built up, this ceased to be a challenge.
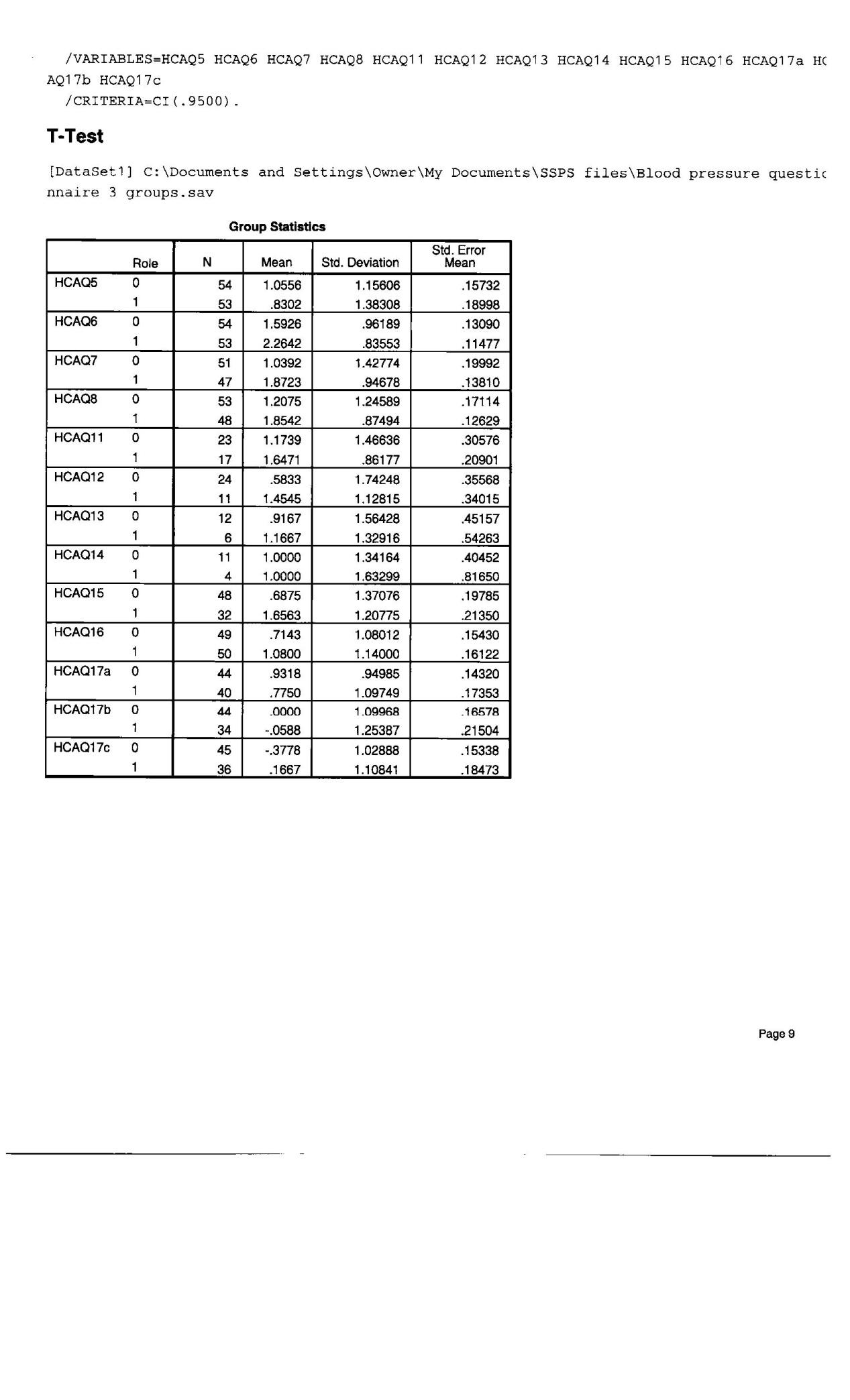
Evaluation Report-A study
A published evaluation report showed that the project might have contributed to a 32% reduction in falls, 60% reduction in fractures and 7% reduction in hospital admissions resulting in a better quality of life for service users, and significant savings in direct and indirect health and social care costs. The call-out rate for the patients’ General Practitioners (GPs) also reduced by more than 85%, leaving the GPs with more time to spend with patients at the surgery. Quite indirectly, these savings more than compensated for the costs of providing the service and should be of interest to Practice-Based Commissioning groups. The service would become even more efficient and effective when the pharmacists involved are qualified as pharmacist independent prescribers.
Independent nurse prescribing by the pharmacist in sexual health services also has great significance. The sexual health services of the United Kingdom are a key priority for the National Health Services (NHS), with sexually transmitted infections and HIV cases continuing to rise. At present, there are around 80,000 people living with HIV in the UK, with annual growth in diagnoses between 7,000 and 8,000. It is also estimated that close to 30% of people with HIV are unaware that they carry the virus. The advances in the treatment of HIV mean that patients are able to live normal lives and have a normal life expectancy which, with the associated conditions of older age, will lead to much greater numbers of patients with complex prescribing needs. Ensuring that the patients are able to discuss their medical therapy and be proactive on their own care is an essential component of HIV care, where patients must be compliant with at least 95% of doses to ensure that the drug has maximum efficacy. Poor adherence and increased drug resistance ultimately lead to the patients requiring newer and highly expensive anti-HIV agents. The pharmacists in an independent prescribing role also play a crucial part in the Nurse independent prescribing in primary and secondary care related to dermatology ailments. Dermatology is one of several clinical areas that are rightly placed to use the expertise of specialist nurses and pharmacists with a prescribing qualification. The long-term, and often visual, nature of dermatology conditions and ailments means that many patients benefit from the person-centered care that caters for both their physical and psychological needs. Increasing demands for several services, for example from higher rates of skin cancer and allergic conditions – highlighted in the NHS Plan – have placed greater demands on prompt access to dermatology services across England.
Role of the pharmacists in Nurse independent prescribing in the community and outpatients
The role of the pharmacists in Nurse independent prescribing in the community and outpatients especially related to epilepsy holds some special significance. Epilepsy is a very common chronic disabling condition of the nervous system, which affects nearly one in 30 people at some time in their lives. Approximately 1,000 people die every year as a result of epilepsy, of which 500 deaths are sudden or unexplained. According to ‘Nice Guidelines ’, epilepsy specialist nurses should be an integral part of the network of care of individuals with epilepsy. Their crucial roles are to support both epilepsy specialists and generalists, and thus ensuring continued access to community and multi-agency services, and provide information, training and support to patients, families and carers. The National Sentinel Clinical Audit of Epilepsy-Related Death found out that 20% of adults and 45% of children with epilepsy as having inadequate medicines management. The report also recommended that all patients should be reviewed annually as a minimum, together with access to a specialist nurse. The Patients with unstable epilepsy such as prolonged or frequent seizures need immediate attention to their medication so as to reduce the possible harm to the patient, as well as the disruption to their daily lives and the possible consequences of a poorly controlled medical condition. Being able to customize the medicines regimens to an individual patient’s condition minimises the risk of side effects and increases efficacy, thereby making it much more likely that the patients can continue to work and look after their children. The Reviews of medicines of the patients and the subsequent follow-up prescribing system can enhance the patient compliance and quality of life; for example, by addressing formulation, frequency of dosing and side effects.
The existing program of the NHS in England: ‘The Operating Framework 2008/09’ to deliver 48-hour access to genitourinary medicine (gUM) clinics means that these services may need to increase capacity. Using the existing staff of the pharmacists with enhanced qualifications and skills may help the NHS to achieve this objective.
In Great Britain, the skills and competencies of non-medical health professionals are increasingly being used to improve patient access to medicines and to reduce doctors’ workload (Stewart 2010). The final Crown Report in March 1999 proposed that non-medical health professionals should be permitted to take on additional prescribing responsibilities. The report defined two new types of prescribers: the independent prescriber and the dependent prescriber. The Health and Social Care Act 2001 (Section 63) allowed for the introduction of dependent prescribing (implemented into practice as supplementary prescribing) status for non-medical health professionals, including pharmacists. Pharmacists with at least two years’ experience as a pharmacist can undertake SP after training at a higher education institution (200 h at the degree/masters level over 25 days) and completing a ‘period of learning in practice’ (PLP) (supervised training under a designated medical practitioner for a minimum of 12 days) in accordance with the curriculum and assessment methods specified by the Royal Pharmaceutical Society of Great Britain (RPSGB). Pharmacists working in various practice settings across Great Britain have been practising SP since March 2004. Published research on pharmacist prescribing is limited to the views of pharmacists from various practice settings and anecdotal experiences of the SP course and the implementation of SP. No national study has been published reporting the experiences of pharmacists relating to their SP course and implementation of SP. Such a study is critical to optimise future training programmes for pharmacist prescribing. Understanding perceived challenges to and benefits of SP implementation could inform policy makers, organisations considering implementation of SP service and pharmacists planning to undertake prescribing training. This study has explored the experiences and perceptions of early pharmacist supplementary prescribers in Great Britain. SP has been regarded as highly beneficial for both patients and pharmacists. Several logistical and financial barriers hindering the implementation of SP have been identified.
New Community Pharmacy Contractual Framework
Background Medicines are the most commonly used form of healthcare treatment. They provide relief from everyday ailments to life-saving interventions for acute illness as well as support for people with long term medical conditions such as asthma, or progressive illnesses such as arthritis or multiple sclerosis. Building on the NHS Plan, in 2003, the Department of Health (DH) set out its intention to increase the public’s choice of when, where and how to get medicines by: freeing up restrictions in England on locations of new pharmacies in the Government’s response to an Office of Fair Trading report: easing bureaucracy around repeat prescriptions; expanding the range of medicines that can be provided without prescription; promoting minor ailment schemes in pharmacies; increase the range of healthcare professionals who can prescribe. Many of these changes will be implemented through increasing the contribution that community pharmacists make to primary health care.
According to the new pharmacy framework, there are three stages of services namely, essential, advanced, and enhanced services. These three services are explained in the ensuing paragraph. Essential services are defined as those services that must normally be provided. Essential services include dispensing, repeat dispensing, disposal of medicines, promotion of healthy lifestyles, and provision due to these errors. These include motion of self care for patients with minor ailments and signposting for patients to other healthcare provision. Advanced services are those which require accreditation of the pharmacist providing the service (such as medicine use review) and/ or specific requirements to be met in regard to premises, such as private consultation areas. Enhanced services are local services such as minor ailment schemes and supplementary prescribing that will be commissioned by Primary Care Trusts, according to the needs of the local population.
Payment will be increasingly directed towards quality, not just dispensing volume, recognising that the pharmacies need a fair return for the services they provide. Medicines Legislation Act in the UK: The Medicines Act 1968 and Council Directive 2001/83/ EEC control the sale and supply of medicines. Once the medicines are authorized, they attain a legal significance. There are three classes of medicine: A new medicine is usually authorised as prescription only (POM). After some years use, if adverse reactions to it are few and minor, it is possible that it may be used safely without a doctor’s supervision. In situations where it is observed that ample safety is being taken, the medicine is authorized for sale by a pharmacist. Similarly, pharmacy medicines which have been safely used for several years may be reclassified for general sale (GSL). The Committee on Safety of Medicines plays an important role in reclassifying the medicines. In cases where reclassification is considered to be safe, public opinion is sought through the portal of MHRA.
Contractual Framework and its focus on the changing role of pharmacies: Community pharmacies are where most people have access to pharmacy services and where 73% of active pharmacists work. A new contractual framework between community pharmacies and the NHS was introduced in April 2005. While the old system emphasised the volume and throughput of prescriptions, the new framework focuses on the range of services that pharmacists provide for patients. These are divided into three levels – essential, advanced and enhanced. Prior to the new community pharmacy contractual framework, the granting of contracts to pharmacies to dispense NHS prescriptions was subject to the NHS (Pharmaceutical Services) Regulations 1992. Since the NHS accounts for the vast majority of all prescriptions, it is difficult for a pharmacy to run a viable business without such a contract. This effectively amounted to full regulation of market entry for new pharmacies. The Government wanted to offer patients more choice in where they get their prescriptions dispensed by making it easier to open new pharmacies. In 2004, it announced new rules to introduce criteria of competition and choice to the regulatory test, exempting the following types of pharmacies from the test: those in areas where consumers already go, such as large shopping developments; pharmacies intending to open for more than 100 hours a week; those in large one stop primary care centres; and internet and mail-order pharmacies that allow people to have medicines delivered to their home. The Government’s commitment to make medicines more readily accessible raises issues including access to medicines, the role of pharmacists, and access to patient information and pharmacies.
Who’s who in Community Pharmacy?
The Royal Pharmaceutical Society of Great Britain (RPSGB) is the regulatory and professional body for pharmacists. The primary objective of the Society is to lead, regulate and develop the pharmacy profession. National Pharmaceutical Association (NPA) is the national body representing Britain’s community pharmacy owners. UK’s Royal College of General Practitioners (RCGP) supports and motivates the general practitioners to attain and uphold the standards of their profession to their utmost levels. The Pharmaceutical Services Negotiating Committee (PSNC) represents community pharmacy on NHS matters. It negotiated the new pharmacy contractual framework with the DH and NHS Confederation.
The British Medical Association’s General Practitioners Committee (BMAGPC)
The BMA represents doctors from all branches of medicine all over the UK. Its GPC represents all GPs, to promote general practice and to protect its fundamental characteristics and interests. Medicines and Healthcare products Regulatory Agency (MHRA) is the executive arm of the UK’s Drug Licensing Authority and is responsible for all aspects of the regulation of medicines in the UK. The Committee on Safety of Medicines (CSM) is an expert Committee that advises the Government on the safety, quality and effectiveness of medicines.
It is widely agreed that there are advantages to making more medicines available without prescription. However, some groups have expressed concern about how far this should be taken. The recent reclassification of a low dose of statin (simvastatin), a medicine that reduces cholesterol levels, is a case being analysed. Statins are currently prescribed to 1.8 million people. In 2004, the Committee on Safety of Medicines (CSM) advised that simvastatin should be available without prescription in a low 10 mg dose, but continue to be available as a POM to high-risk patients. RPSGB welcomed the decision. It believes that there is a clear public health benefit to be gained from making this medicine available without a prescription. However, others including RCGP, BMA GPC and the consumer organisation, disagree. BMA GPC is against the introduction of statins to the over-the-counter market for a range of reasons, including safety concerns. It suggests that even low doses can cause side effects, such as muscle damage, and thus considers it inappropriate to provide such medicines without a doctor’s supervision. Such safety concerns should be addressed by the CSM when it is considering its advice on an application to reclassify a medicine. Neither MHRA nor the CSM publish a report of the evidence considered and why their decision was reached. Some have questioned the benefits of wider access to medicines in general and to preventative medicines in particular. While the reclassification of simvastatin has been welcomed by the RPSGB, the medical profession has expressed doubts over the balance between safety and efficacy. For instance, the RCGP points out that the therapeutic benefit of 10 mg of simvastatin (a 27% reduction in risk of heart attack and stroke) only applies to those people at increased risk of heart attack or stroke in the first place. It is concerned that people taking the drug who are not at increased risk of stroke or heart attack may receive no therapeutic benefit while exposing themselves to the risk of side effects. RCGP is concerned that, in practice, it will be the ‘worried well’ who take preventative medicines rather than the people who may benefit most from them. It is worried about the psychosocial implications of an ever greater proportion of the population considering themselves to have some sort of health problem. DH argues that by extending access to such medicines it is giving people more choice about how they protect their health. Consider that patients who have a clinical need to take medicines such as statins should be able to take them on the NHS. Pharmacists are experts in the use of medicines and must complete a four year degree and one year’s practical training to qualify. It is widely agreed that better use could be made of pharmacists’ skills and knowledge; the new pharmacy contractual framework sets out the Government’s plans on how to achieve this. Because community pharmacists operate within a commercial environment, questions have been raised about whether they are best placed to decide if a patient requires a medicine and if so, which one? However, one of the key responsibilities within a pharmacist’s code of ethics is to act at all times in the best interests of the patient. Pharmacists are expected to assess whether a prescription or an over-the-counter medicine is appropriate. The public appears comfortable with a pharmacist’s dual roles of retailer and healthcare professional. In a survey more than half the respondents disagreed with the assertion that pharmacists sometimes recommend products that are not strictly necessary in order to make a sale.
New Schemes
Over the past five years a number of schemes have been established to better integrate pharmacists into primary care and the new contractual framework will further encourage this. In general these schemes have been considered a success and have been integrated into the new pharmacy contractual framework. They offer easier and faster access to services for people as well as reducing a GP’s workload. For example, the Care at the chemist scheme in Bootle resulted in a reduction in GPs’ minor ailment workload from 8.9% of consultations to 6.6%. Repeat dispensing by pharmacists is also likely to reduce GPs’ workloads. Currently about 75% of GPs’ prescriptions are for repeat medicines. Pharmacists can offer medicines usage review as an advanced service under the new contract. Here, pharmacists undertake a review (of both prescribed and non-prescribed medicines) with patients receiving medicines for long term conditions, to establish a picture of their use of the medicines. It is anticipated that this will help patients to understand why the medicines are prescribed for them, as well as identifying side-effects that they may be exposed to. Medication review and management can be complex as many older patients receive treatment for at least four different conditions, leading to concerns about how different drugs interact with each other. RCGP has thus questioned whether pharmacists’ training and access to patient records are sufficient to enable a safe review. However, the DH points out that pharmacists training does include drug interactions, and that there is evidence from pilot schemes that pharmacists can carry out medication reviews effectively. Furthermore, to be able to offer this service under the new pharmacy contractual framework, pharmacists must be accredited and will have to provide a report of the review to the patient’s GP.
Supplementary Prescribing and the Better use the Pharmacists’ Skills
Minor ailment schemes have included treatment for conditions such as athlete’s foot, earache, constipation, hay fever and cystitis. The interventions available to a pharmacist are usually of three main types: advice only; advice and supply of medicines over-the-counter; or referral to a GP. In the Care at the chemist scheme in Bootle patients requesting a GP appointment for minor ailments, such as earache, nasal symptoms, and cough, were offered a consultation at a pharmacy. 38% of patients were happy with this option and thought the arrangement was convenient. Patients who had not had the symptoms before preferred to see a doctor.
Supplementary prescribing, including repeat prescribing, is a sort of cooperation between a General Practitioner who assesses a patient’s ailment, another medical practitioner who monitors the patient and prescribes further supplies of medicines within an individual clinical management plan, and the patient who agrees to the supplementary prescribing arrangement. All pharmacist supplementary prescribers must undergo additional training, including a period of supervised practice. In a diabetes shared care scheme, GPs were able to refer patients with type 2 diabetes back to a pharmacist-led outpatient-clinic if complications developed. The pharmacist reviewed their treatment, altered their medicines according to laboratory results and offered patients advice and information. None of the patients in the shared care scheme were readmitted to hospital with diabetic complications in contrast to 25% of the patients in the control group. In a study of repeat prescribing in Dundee 81% of patients preferred it to the traditional system of requesting a prescription from their GP.
Usage of IT by Pharmacist
Information technology will play a fundamental part in helping pharmacists to provide new services. According to the National Pharmacy Association, the Royal Pharmaceutical Society of Great Britain, and the Pharmaceutical Services Negotiating Committee, the pharmacists should have more admittance to information pertaining to the patients so that they are able to offer secure and efficient service. The National Programme for IT including the NHS Care Records Service and electronic prescription service, from GPs to pharmacists, will address this. Over time the benefits of the electronic prescription service will include: increased safety; more choice and convenience for patients; better information for prescribers and dispensers on which to base clinical decisions; and reduced administrative burden in GP practices and community pharmacies. However, the NHS Care Records Service is not due to be fully implemented until 2010. Therefore, in the meantime, continuity and completeness of patient care will require good communication between GPs, pharmacies and the patient. Discussions as to what levels of access to patient information a community pharmacist may need are ongoing. The consumer group suggests that patients are likely to be more comfortable with community pharmacists having access to their NHS records where there is an existing patient-pharmacist relationship. Attitudes towards any pharmacist or pharmacy technicians and assistants having access are less certain. The new NHS IT infrastructure makes provision for restricting the information available to a healthcare professional depending on the service that the professional is providing. In addition, pharmacists are bound by their code of ethics to respect patient confidentiality. DH is planning to hold a consultation about pharmacists’ access to patient information.
Competition and community pharmacies
In 2003 the Office of Fair Trading (OFT) advised that the pharmacy sector should be deregulated. It suggested that relaxing the rules on where pharmacies can be located, including allowing internet-only and mail-order pharmacies, would save patients and the NHS money. The House of Commons Health Select Committee considered OFT’s recommendations but was not in favour of deregulation. The Committee considered that the OFT report had failed to take account of the wider role of pharmacies within the NHS. Similarly, the Government did not back a move to a fully deregulated system, but favoured opening up the market in England to more competition and choice. It announced new rules to do this in 2004. Reform of the NHS (Pharmaceutical Services) Regulations 1992 will allow market entry exemptions for large shopping developments, pharmacies opening more than 100 hours a week, large one-stop primary care centres and internet and mail-order pharmacies. The National Pharmaceutical Association (NPA) is concerned that some local community pharmacies will not survive such competition. It suggests that this could potentially lead to reduced availability and access to local services. Parliamentarians have also expressed concern that the changes do not fit with the Government’s plans to enhance the role of community pharmacies.
Pharmacists and their role in sales of medicines on the Internet
With the advent of new technologies and the internet, a new way of doing business has come into being. Prior to this, business, as usual, was done through shops. There were some products that could be ordered through mail but the quantum of such products was negligible. But thanks to the internet facility, now even pharmacies can have their own websites through which they can cater to the global customers. The following are the benefits of having a personalized website for pharmacies:
- By having an own website and uploading it through a reliable Search Engine Optimization (SEO) company, pharmacies can have a larger market base.
- The pharmacies can cater to mail orders throughout the world.
- The pharmacies can promote their specialities or expertise in any particular field to the worldwide public.
- It is very easy for pharmacies to be in contact with other businesses and the customers.
- It is a very cost effective way of doing business.
- The pharmacies can surf the internet in order to search for better and less costly drugs or their substitutes.
- The pharmacies can update their data by having information on the latest inventions of drugs and/or diseases and their cures.
- The pharmacies can have information on any scheduled or ongoing conferences and can apply for registration.
Buying medicines online or by mail-order offers potential benefits – for example to house-bound patients or those with an embarrassing health problem – and is likely to become increasingly popular. Internet sales can broadly be divided into legal and illegal. Illegal sites offer POM without a prescription. Predominantly they offer ‘lifestyle’ drugs such as Viagra (sexual dysfunction) and Xenical (weight loss). The MHRA Enforcement unit attempts to close down such sites but as many are based outside the UK they fall outside MHRA’s jurisdiction. Distinguishing legal from illegal sites is a major issue for customers. POM and P medicines should only be taken in consultation with a healthcare professional, in order that the appropriate product is prescribed; any side effects are carefully monitored and other medicines and treatments taken into account. As the advent of internet and mail-order pharmacies allows this interaction to take place remotely, the patient needs to be sure they are communicating with a qualified, registered professional. Likewise, the professional needs to be certain that they know the patient they are communicating with. RPSGB has set up a working group that includes government and other interested parties, to consider how the regulatory framework can be enhanced to provide adequate safeguards for people purchasing medicines on-line. The group will consider the need for an information campaign to increase public awareness and is expected to report within the coming year.
The Government is committed to expanding the role of pharmacists and making medicines more widely available to the public. The medical profession is concerned that increasing access to preventative medicines via reclassification may target the ‘worried well’ rather than those most likely to benefit. It is widely agreed that better use could be made of pharmacists’ skills and knowledge. The new pharmacy contractual framework should enable this, leading to easier and faster access to services for patients as well as reducing GPs’ workloads. Making the medicines more readily accessible raises the issues such as the role of pharmacies, pharmacist’s access to patient information, and access to pharmacies.
Introduction: PEST Analysis of Community Pharmacy
In recognition of the need for change in an industry it is important to consider the strategic position of the industry, whether it is in decline or growth compared to the wider market. Other factors which will influence the need for change consist of changes to the legal framework and social environment in which the pharmacy industry operates. Two most commonly favoured methods of analysing the business environments are SWOT analysis (The Strengths, Weaknesses, Opportunities, and Threats) and the PEST analysis (Political, Economical, Social, and Technological factors).The PEST analysis tool has been developed to assist with strategic business planning by allowing a macro-environmental assessment of trading to be examined. PEST analysis takes into consideration the Political, Economic, Social and Technological influences on the industry. The Political factors for most industries are restricted to legal changes, taxation and tariffs set by the Government, but in the case of pharmacy the Government influence extends into the economic factors. Other political factors affecting the community pharmacy are the laws of employment and the stability of the government. The economic factors responsible for the performance of a community pharmacy include the financial growth of the country or state, the rates of interest applicable, the prevailing rates of exchange and the rate of price increases. The Social factors represent changing customer and trade behavioural trends. Customer behaviours include the people being conscious about their wellbeing, the increase in population and the importance of safety that they have. Technological factors consider how innovation in practice using new processes and equipment will require change. The research and development activities being carried out make a lot of difference. By having an up to date R&D facility, pharmacies can keep up with the pace of development and the inventions being made in the field of pharmacy. The main factors influencing the need for change in the pharmacy profession have been given below:
Table 1: PEST Analysis of Community Pharmacy
Government Policies
Medication supply to patients in the United Kingdom comes under the legal regulation with pharmacies supplying the majority of the population. Pharmacy is an independent healthcare profession with its own representative and regulatory organisations. Since the establishment of the National Health Service the Government through the Department of Health has been the main customer for pharmacy services. The Department of Health of the UK determines the changes to the legal basis of medicines supply and in consultation with the Pharmacy Services Negotiating Committee, representing the pharmacy contractors, sets the remuneration levels for pharmacies contracted to the National Health Service. As dispensing volumes increased in the United Kingdom pharmacists have found it impossible to dispense all prescriptions unaided. It therefore became necessary to use supporting staff that have usually been taken from a medicine sales role to assist in dispensing prescriptions. Informal dispensary support members of staff have with appropriate training become qualified as “dispensers”, equivalent to the National Vocational Training Level 2. On completion of further training to National Vocational Training Level 3 dispensers can qualify as “dispensing technicians”. Professional registration at the dispensing technician level is now being encouraged and will soon be a statutory requirement. At present, community pharmacy practice requires that a pharmacist is able to supervise the activity of staff in making sales of medicines to the public or in dispensing prescriptions (Department of Health 1968). Technological changes necessitated by the introduction of computers and private video transmissions have made it possible to provide a level of supervision by a pharmacist from a remote location. The introduction of responsible pharmacist legislation enables the pharmacist to be absent from the pharmacy for up to two hours a day (Anon 2008). The legal supervision of medicine sales or supply still requires the personal presence of a pharmacist in the community pharmacy although this situation may change as a result of future legislation. A potential effect of remote supervision of community pharmacies could be that several low dispensing volume pharmacies could be supervised by a single pharmacist. If this does become an accepted model of pharmacy practice there would be a serious impact upon pharmacist employment.
The new community pharmacy opening has been restricted under the terms of the pharmacy contract regulations unless a pharmacy is open for one hundred hours a week. The supermarket groups in the UK had lobbied with the government for the right to operate pharmacies from within their stores for several years leading to an official review which recommended removal of controls {The Office of Fair Trading, 2003 13 /id}. A compromise for allowing all supermarkets to incorporate pharmacies was to require these supermarket applications to dispense to succeed if extended hours were offered thereby increasing public access to pharmacy services {Advisory Group on the reform of the NHS (Pharmaceutical Services) Regulations 1992, 2004 14 /id}. If it is assumed that a standard pharmacist is working forty hours in a week, these one hundred hour pharmacies would require two and a half full time equivalent pharmacists to supervise their operation. Unless the supermarket is located close to a doctor’s surgery it is unlikely that hourly prescription volumes will be high. The prescription volumes in the periods when the doctor’s surgeries are closed probably do not justify the presence of a pharmacist if it were not a contractual requirement. Remote supervision of these hours worked by the pharmacists would represent a major economy for the supermarkets and would reduce employment options for community pharmacists.
In a recent consultation document, the Government wanted to consider changes to pharmacy practice that might incorporate a move to dispensing technicians having a greater role in the supply of medicines under the “remote supervision of pharmacists” (Department of Health 2004). Pharmacist supervision of medicine dispensing has been an area of concern to the profession since a review (Nuffield Foundation 1986) following which it has generally been considered that for a pharmacy to be open required a pharmacist to be present. With the recognition of the dispensing technician qualification and registration of technicians, there has been concern that the Government would change the supervision rules. It is thought there may be changes planned to permit a pharmacy to operate with qualified technicians performing the dispensing roles with access to an offsite pharmacist to assist when necessary (Axon 2007). A willingness by Government to examine how other European Countries supply prescription medication could eventually lead to reduced pharmacist involvement in dispensing as some countries allow unsupervised technician dispensing (Department of Health 2004). Economically, pharmacy as a profession is in a weak position as the main customer for its professional services is the Government in the form of the National Health Service. The contract to supply prescription medicines under the National Health is on the basis of the cost of the medication plus a professional fee (Anon 2009b). This remuneration scheme allows the Department of Health to set an annual ‘global sum’ for community pharmacy payments which represents the profit element for supply of National Health Service prescriptions or services. After allowing for a basic practice fee to reward the public health advisory role and any additional pharmacy contract services the balance of the global sum is divided by the anticipated number of prescriptions dispensed to obtain the annual professional fee per prescription item. The remuneration system for prescription item costs is adjusted to allow for discounts obtained in purchasing medicines for supply on prescription from pharmaceutical wholesalers. Since the introduction of discounts on pharmacy accounts by the wholesalers the Department of Health has applied a deduction to avoid paying pharmacies above the actual ingredient cost plus a dispensing fee. This “cost plus” fee basis allows the Department of Health to reclaim any profits made from more efficient drug purchasing by community pharmacies. As discounts vary with the account value, the deduction of the Department of Health, changes from 5.63 percent, for less than 126 prescription items a month, to 11.5 percent for pharmacists dispensing 160001 or more items a month (Anon 2009b).
Profits through purchasing drugs at a discount or buying at a lower cost than that paid by the Department of Health to pharmacies are reclaimed following annual discount enquiries which compare costs expected by the Department of Health with actual prices paid by pharmacies (Anon 1999). When new trading opportunities occur, as in the example of parallel imported medicines (branded drugs sold in continental Europe at prices below UK wholesale prices and imported outside the normal wholesale system historically used by pharmacies) can make significant profits for community pharmacies. However, after a period of increased profitability the prices paid by the National Health Service are discounted to reflect real costs and following a discount enquiry the excess profits are reclaimed.
The Department of Health effectively controls the level of profit that can be made from dispensing services since it sets the global sum for pharmacy remuneration and this could be a threat to future pharmacy profitability if the global sum is reduced. Declining profits could result from future Government spending reductions as the Department of Health could be facing significant cuts (Sylvester, Thomson, & Elliott 2009).
The pharmacy contract has undergone few changes since the establishment of the National Health Service but was substantially changed by the New Contract in 2004 {Department of Health, 2003 12 /id}. This new contract has divided pharmacy services into core, advanced and enhanced services. Core services revolve around the medicines supply role and account for approximately ninety nine percent of professional income {Carroll, 2010 11 /id}. The dependence on dispensing is such that due to the decline of over the counter sales between 90% and 95% of the income of an average pharmacy is generated by the National Health Service contract {Advisory Group on the reform of the NHS (Pharmaceutical Services) Regulations 1992, 2004 14 /id}.
The newly introduced advanced and enhanced services require the use of more clinical skills by the pharmacist but so far have not provided a significant financial reward. Funding for additional advanced services is included within a total remuneration, or ‘global sum’, of payments for National Health Service contracted pharmacy services. A future ‘new medication service’ will be made available as an advanced service potentially capable of increasing income for community pharmacies by £55 million a year. However, it appears to be at the expense of core service funding as the introduction of this service is not expected to increase the cost of pharmacy contract services to the National Health Service {Alexander, 2011 12 /id}. Additional funding pressure results from the expectation by the Department of Health to be capable of year on year efficiency savings, as can be seen from the expectation that £110 million would be saved from the pharmacy global sum if the new medication service had not been introduced (Alexander, 2011 12 /id).
This financial pressure on core services could lead to the adoption of technologies which would reduce pharmacist involvement in the dispensing process {Roberts P, 2004 ROBERTSP2004 /id}. There is a threat to community pharmacist employment as a reduction in pharmacist time supervising dispensing could potentially reduce community pharmacist numbers if additional roles are not adopted and adequately remunerated. In order to increase community pharmacy professional income in the future it appears it will be necessary to extend professional practice beyond that covered by the standard pharmacy contract.
Value of OTC medicines
The value of OTC medicines and traditional pharmacy goods sold from pharmacies has declined over the second half of the 20th century as retail trade has gravitated towards supermarket shopping (Defra 2006). The pharmacy sector has also seen an increase in corporate ownership as a few multiple chains, the largest being owned by pharmaceutical wholesalers, have come to monopolise the retail sector (Tann and Blenkinsopp 2004). Supermarket chains have in recent years increased the range of items sold to include traditional pharmacy goods, cosmetics, baby food and over-the-counter medicines, reducing sales from community pharmacies despite an overall increase in retail sales in the country. This loss of sales has increased as supermarket chains are now incorporating their own pharmacies into their stores, thus taking ‘pharmacy only medicine’ sales away from traditional high street pharmacies.
The pharmacy profession was based on the compounding of medicines for supply to the public either on a doctor’s prescription or through recommendation by the pharmacist. However, the practice of pharmaceutical compounding skills has become increasingly irrelevant in the 21st century. Medical research has led to the adoption of ‘Evidence-based medicine’ increasing the use of treatments that research can prove to be both effective and safe. Evidence-based medicine seeks to utilise the most effective medication available based upon the results of modern research methods to remove individual clinician bias. Traditional medications in contrast have been prescribed based on the experiential prescribing of individual clinicians without the advantages of unbiased scrutiny.
The use of traditional compounded medicines has therefore declined as few of these products have ever been subjected to scientific review of efficacy. Some compounded medicines are described as being less suitable for use in the national prescribing guidance handbook, the British National Formulary, and this has further reduced the prescribing of these products (Anon 2008b).
During the 1980’s dispensary computer systems were adopted by community pharmacies for prescription labelling, stock control and recording patient’s medication records. Early experiences were based on the Apple II, and BBC microcomputer systems with the software loaded daily from a floppy disk. The ability to word process labels and the introduction of patient ready packs of medicines, medicines pre-packed in standard dispensing quantities with patient information leaflets, made repeat dispensing a dispensary assistant staff role. These dispensary assistants have evolved into dispensing technicians who are now being required to register in a similar way to pharmacists (Department of Health 2009). Newly developed drugs have normally been formulated into unit dose medicines which are themselves packaged in patient ready packs usually representing either a course of treatment or for more long-term treatments one month supply. This standardisation of packing has led to the development of computerised robotic dispensing systems which can rapidly select and label prescriptions (Swanson 2009).
When the electronic transfer of repeat prescriptions from doctors to pharmacies is operational, the use of robot dispensing systems may make dispensing a largely automated process. This automation already poses a threat to future employment of both pharmacists and dispensing technicians with one hospital pharmacy finding a reduction of 32 per cent pharmacist hours and 52 per cent dispenser hours required to perform the medicines supply function for their patients following the introduction of robotic systems (Roberts & Gray 2004).
In the second half of the 20th century there were changes in the practice of hospital pharmacy which led to the development of an enhanced clinical function with ward-based roles. Pharmacists started to advise the medical profession on medication, becoming recognised experts on drug therapies. To allow pharmacists to perform the new clinical roles many of the dispensing duties were delegated to suitably trained and qualified (dispensing) technicians.
In community pharmacy change has been more difficult to achieve. The profession’s core income is from dispensing services and for significant change to occur there is a requirement for the remuneration system to be changed. In the 1980s the Government commissioned a study to review the pharmacy profession and suggest future developments (Nuffield Foundation 1986). The profession was considered to have a potentially major role in self-medication and health education but needed to improve pharmacy staff training. While changes were made to the dispensing contract to recognise these roles the professional’s financial reliance remained on dispensing services.
The development of more clinical roles occurred at about the same time as the lengthening of the pharmacy qualifying degree to four years. This could potentially produce graduates with greater clinical knowledge (although ways to increase clinical education are still under review (Department of Health 2008)) and help engender a desire to practice in more patient orientated roles. Concern over the development of the profession among the pharmacist community led the Royal Pharmaceutical Society in 1995 to initiate a discussion process, ‘Pharmacy in a New Age’ (Longley 2006). A widespread dissatisfaction with the lack of professional development since the Nuffield report and a previous unwillingness to change entrenched practices was identified (Parkin 1999).
Prescribing errors – A concern and a research study
Studies carried out in the American hospitals suggest that prescribing errors occur in 0.4–1.9% of all medication orders written and cause harm in about 1% of all inpatients (Emmerton , Marriott, Nissen, & Dean 2005). No large scale studies of prescribing errors have been carried out in the UK, although studies of pharmacists’ interventions suggest that many errors occur and are subsequently remedied following the interventions of ward pharmacists. A recent report from the Department of Health recommended that serious errors in the use of prescribed drugs should be reduced by 40% by 2005, and that baseline rates of errors will need to be established. However, a major problem with interpreting quantitative prescribing error studies, is that the definition of an error used by the researchers is often ambiguous or not given at all. Comparisons of error rates across the literature are therefore accompanied by significant uncertainty. Where definitions are given, there may be marked divergences among studies. A common approach has been to consider that a prescribing error has occurred if both doctor and pharmacist agree that this is the case. While pragmatic, this approach is limited by potential divergences in the knowledge and views of individual practitioners. Other studies have used outcome-based definitions, including as errors only those that result in harm to the patient. However, in many cases, pharmacists intervene to prevent errors from reaching the patient and so the outcome remains unknown. Even where prescribing errors are defined more explicitly, there is wide variation in the types of events included. For example, Betz and Levy include “prescribing a medication without sufficient education of the patient on its proper uses and effects” while Tesh et al include “the prescription of medication by brand (instead of generic) name”. Others do not consider these to be prescribing errors. Consequently, it is almost impossible to compare data from divergent studies or to use prescribing error rates as a meaningful component of clinical governance. If alternative prescribing systems are to be evaluated in terms of their effects on prescribing error rates, a clear definition is needed. Thirty four (79%) of those approached agreed to take part. These comprised nine physicians, three surgeons, 12 pharmacists, seven nurses, two clinical pharmacologists, and an anaesthetist. A wide range of clinical specialities were represented; nine of the panel had extensive experience of medication error research and one was the editor of a relevant peer reviewed journal. In the first Delphi stage, responses were received from 30 (88%) of the 34 judges. Responses to the second stage were received from 26 (87%) of the 30 judges to whom second stage questionnaires were sent. When asked for their opinion on the definition proposed, the judges’ median score was 7.0 and the inter-quartile range 6.5–8.0. This indicates that the consensus was to accept the researchers’ preliminary definition. Many additional comments were made relating to this definition, most of which fell into three categories. Firstly, four respondents were unsure whether errors in the prescribing decision should be included as well as those in the prescription writing process. These judges considered the prescribing decision to be part of a broader concept of “clinical decision making” rather than “prescribing”. However, other respondents emphasised the importance of including both elements of the definition, and it was concluded that both should remain. Secondly, six judges were concerned about the use of the word ‘significant’ and considered that the inclusion of this word meant that the definition was only of a “serious” prescribing error. However, others felt that this word should be included for two reasons:
- it was considered important to differentiate between clinically meaningful prescribing errors and those cases where some optimisation of treatment was possible but where a prescribing error could not be said to have occurred;
- it was recognised that cognitive errors could occur in the prescribing process without there being any adverse consequences for the patient.
For example, a doctor may prescribe drug X instead of the intended drug Y, but if both are equally safe and effective then the cognitive error is not clinically important. It was therefore considered that the word ‘significant’ was necessary, but that it should be made clear that the definition is of a “clinically meaningful” prescribing error. Finally, three judges indicated that a comparator was needed within the definition as “reduction” and “increase” implied a baseline. It was therefore decided to add a statement to this effect. The definition of a prescribing error finally adopted was therefore: “A clinically meaningful prescribing error occurs when, as a result of a prescribing decision or prescription writing process, there is an unintentional significant reduction in the probability of treatment being timely and effective or increase in the risk of harm when compared with generally accepted practice”. Using the Delphi technique, a general definition of a prescribing error has been developed together with guidance concerning the specific types of event that should be included. This is practitioner led, more detailed than the definitions used in previous studies, and concordant with human error theory. According to theories of human error, a series of planned actions may fail to achieve their desired outcome because the plan itself was inadequate or because the actions did not go as planned. Our definition reflects this distinction while including failures in the prescribing decision as well as the prescription writing process.
Pharmacy in New Age
The ‘Pharmacy in a New Age’ discussions also led to the understanding that without government support and encouragement improvements in community pharmacy practice would not be achieved (Longley 2006). The willingness to change expressed by the profession empowered the Pharmacy Services Negotiating Committee and the Department of Health discussions. These discussions produced a new pharmacy contract which could reward new non-dispensing services and reflected the aspirations expressed by the pharmacy profession in the ‘Pharmacy in a New Age’ report (Department of Health 2005; Parkin 1999).
The new pharmacy contract introduced in 2005 allowed for three different levels of community pharmacy services (Department of Health 2005). The core dispensing, health promotion and self medication roles were classed as ‘essential services’ to be supplied by all pharmacy contractors (Department of Health 2005a). ‘Advanced services’ could be offered by all pharmacies, subject to specified criteria, offering more clinical services on to a national service specification (Department of Health 2005b). At present there is only one advanced service, the Medication Use Review. The third level of service incorporated in the new contract allows local NHS organisations to commission ‘enhanced services’ to satisfy local needs. Examples of local enhanced services include emergency hormonal contraception and the minor ailments scheme.
The government around this time asked Dr. Crown to review the prescribing, supply and administration of medicines in the UK (Department of Health 1999; Parkin B 1999). Changes were suggested to allow a new category of prescriber, supplementary, who would prescribe for long term conditions under the supervision of an independent, usually medical prescriber. Initially supplementary prescriber status was restricted to suitably trained nurses but training and qualification were extended to include pharmacists.
Non-medical prescribing is an initiative introduced by the National Health Service that was designed to encourage healthcare professionals to expand their breadth of knowledge and to improve positive health-related outcomes for patients (Cooper et al. 2008a). As I have always been interested in increasing my ability to positively influence patient’s health I became the first community pharmacist supplementary prescriber in Dorset. Supplementary prescribing requires the prescriber to treat patients to a Clinical Management Plan which specifies patient condition, drugs to use, referral conditions and requires annual review by the independent prescriber. The Clinical Management Plan is the basis of prescribing practice among the independent and supplementary prescribers. Satisfactory experience with non-medical supplementary prescribing led to the introduction of independent prescribing status for suitably trained non-medical prescribers. In the United Kingdom since the establishment of the National Health Service the administration of medications and drugs to patients has been based on instructions from a doctor or dentist. The legal basis for supply of medicines to the public was regulated by the government (Department of Health 1968). The importance of over the counter medication and the role of the pharmacist in controlling access to some medicines with medicines being classified as being freely available for sale (the General Sales List), available from pharmacies (P medicines) and restricted to prescription (POMs or prescription only medicines).
In response to a global need to increase access to POM medication legal changes have been made by the Department of Health which extended the right to prescribe to suitably qualified members of both the nursing and pharmacy professions (Emmerton et al. 2005). The government found it necessary to introduce prescribing policy changes to increase access to commonly prescribed medicines to reduce the workload of doctors. It was hoped that by allowing non-medical prescribing for patients suffering from long term conditions, doctors would be able to produce savings by reducing the delay on diagnosis of newly presenting conditions.
It was felt necessary to initiate fresh forms of prescribing in NHS methods in order to facilitate health professionals, who were not from the health field, to have the prescription rights. Following lobbying and consultations among the government, the various healthcare professions and concerned patient groups an inquiry was initiated into the issue. Dr. Crown was asked to review the prescribing, supply and administration of medicines in the UK and propose improvements to the current system (Department of Health 1999). Changes were suggested to allow a new category of prescriber, supplementary, who would prescribe for long term conditions under the supervision of an independent, usually medical prescriber. Initially supplementary prescriber status was restricted to suitably trained nurses but, following satisfactory experience with nurse prescribing, training and qualification were extended to include pharmacists.
Non-medical prescribing is an initiative introduced by the National Health Service that was designed to encourage healthcare professionals to expand their breadth of knowledge and to improve positive health-related outcomes for patients (Cooper, Anderson, Bissell, Guillaume, Hutchinson, James, Lymn, McIntosh, Murphy, Ratcliffe, Read, & Ward 2008a). Supplementary prescribing requires the prescriber to treat patients to a patient specific Clinical Management Plan which defines the patient condition, drugs to use, referral conditions and requires annual review by the independent prescriber. The Clinical Management Plan is the basis of prescribing practice among the independent and supplementary prescribers. Supplementary prescribing is based on a three way agreement between the patient, independent prescriber and supplementary prescriber producing a bureaucratic complication to the supply of medicines. Concerns about the limitations of this tripartite model of supplementary prescribing led moves to develop another prescribing model which could encompass all allied health professionals. Allied health professionals felt insufficiently empowered and subjected to restrictions due to the need to implement the clinical management plan approved by their independent prescriber when making prescribing decisions. Satisfactory experience with the prescribing of non-medical supplementary prescribing led to the introduction of independent prescribing status for suitably trained non-medical prescribers.
An example and the research Undertaken
“Independent Prescribing at Highcliffe Medical Centre”
Overview
The case involves a pharmacist at a prescribing role at the medical centre. He had been at work at Highcliffe Medical Centre since 2004, initially as a trainee supplementary prescriber and subsequently as a qualified supplementary prescriber. The person attained the qualification as an independent prescriber in January 2008. Highcliffe Medical Centre practice was a specialist hypertension clinic where the pharmacist prescriber had full access to the patient’s medical records. The pharmacist also worked in the pharmacy based within the Medical Centre and following discussions with the Medical Centre and the local Primary Care Trust, the local National Health Service organisation, performed the new pharmacy contract Medication Use Reviews based at the Medical Centre. In 2005, the National Health Service of the UK introduced a new contract for community pharmacies which recognised three levels of pharmacy service: ‘basic or core services’, ‘advanced services which are commissioned on a national basis’ and ‘enhanced services which are commissioned to fulfil local needs’. The reviews are performed face to face with the patient and aim to increase concordance with treatment plans through improved patient education and identification of adverse effects to prescribed medication. These reviews were performed in the Medical Centre with access to the patient’s medical records and could include when necessary measurement of blood pressure in response to clinical system prompts. In this way, blood pressure recording was incorporated into Medication Use Reviews and for patients taking only blood pressure medication, Medication Use Reviews into hypertension clinics.
Patients are usually referred to the pharmacist following blood pressure measurement by one of the Medical Centre nurses or healthcare assistants in accordance with the practice protocol. When these members of the nursing team found it necessary to have a second appointment to confirm raise blood pressure and increase treatment the pharmacist-led clinic was an alternative to referral to a doctor. A second route for patient referral to the hypertension clinic is following a routine review of patient medical records by one of the Medical Centre doctors. For the Saturday morning ‘workers’ sessions, patients are invited to attend by letter following a review of a clinical system report listing details of time since last review, patient age and last recorded blood pressure. Finally, patients who are seen in Medication Use Reviews by the pharmacist prescriber may have their blood pressure checked if their medical record indicates this is required. If the blood pressure was found to be raised during the Medication Use Review these patients are referred for follow-up to the hypertension clinics.
The monitoring of patient blood pressure is based on the British Hypertension Society’s recommendations (William, Poulter, Brown, Davis, McInnes, Potter, Sever, & Thom 2004) with notice being taken of further needs of the older patients (Scottish Intercollegiate Guidelines Network 2001). Whenever possible the patients are recommended to adopt a healthy lifestyle as this can effectively control the blood pressure for some patients and will reduce cardiovascular risk factors for all patients if adopted. Particular emphasis is put on encouraging a healthy lifestyle for patients known to be tobacco smokers. It is keen on encouraging enrolment in a smoke stop clinic operated by the asthma specialist nurse at the Medical Centre. For all overweight patients, lifestyle advice promoted weight loss to try achieving a normal weight as excess weight is associated with an increased risk of hypertension (Guidelines Committee 2003). Reduced salt, dietary fat (particularly saturated fat), and alcohol intake are encouraged at the medical center for all hypertension patients. To balance these reductions, an increase in physical exercise and intake of fruit and vegetables is promoted to the clinic’s patients as these are believed to be beneficial to blood pressure control (Guidelines Committee 2003). The prescribing practice since qualification has been continued to be guided by the supplementary prescribing clinical management plan agreed with the Medical Centre. The clinical management plan was based on the joint guidelines of the National Institute of Clinical Excellence and the British Hypertension Society (William, Poulter, Brown, Davis, McInnes, Potter, Sever, & Thom 2004). The choice of drugs to prescribe was based on the Highcliffe Medical Centre drug formulary and with the exception of modified-release medication, all prescriptions have been written for the necessary drug by the generic name. The details of patient consultations have been recorded as patients are seen and are available to all the other members of the Highcliffe Medical Centre prescribing team. When it was found to be necessary patients were given follow-up hypertension appointments which were generally made by the pharmacist prescriber as patients were seen. The Patients who cannot be prescribed sufficient medication under the Clinical Management Plan, due to the inability to tolerate a large enough range of treatments and maximum doses are referred to the Medical Centre’s doctors. These patients depending on individual needs and consent may be managed by their doctors on medication not covered by the Clinical Management Plan, be referred for a consultant opinion or if unwilling to follow these options given maximum tolerated treatment and this recorded in their records.
Since qualification as an independent prescriber no major drug prescribing changes have occurred although prescribing practice has been extended to include the adjustment of doses of antihypertensive not covered by the original Clinical Management Plan. In most cases, this has been to either increase or reduce doses of alpha-blocking medication. The only increased range of drug initiation has been to start two patients on centrally acting antihypertensive agents but these prescribing decisions have always been shared with a Medical Centre doctor. The opportunity to extend treatment into the final stages of the British Hypertension guidelines has not resulted in the initiation of additional spironolactone or alpha-blockers during the clinics. Patients who the pharmacist prescriber considered might require this level of treatment were routinely referred to a general practitioner for further management. The general practitioner can then prescribe for the patient or if they considered it appropriate make a referral for secondary care consultation.
Methodologies of the Research
The study will be carried out at the Highcliffe Medical Centre. This section describes the research design, the frame of the research. The methodology is the basic structure of the research. It gives a thorough account of the process of the work at hand. There are exploratory and descriptive research methods from which the suitable type of research methodology is first decided. That is followed by the selection of the process in the chosen method. The hypotheses, that are appropriate to the study, are formulated.
Research Design
Kothari (2004), states that Research design is a plan or a framework for a study that guides to collection and analyze the data. It is the conceptual structure in conducting research with the economy in procedure. It is the blueprint of the work planned by the researcher. It helps the researcher to conduct the research in a well-planned manner Based on the problem selected for research the researcher frames a suitable research design.
Research design designates a plan of action that is to be conducted regarding the proposed work of research. The plan provides guidelines for the research and the process of research. This plan enables the researcher to keep track of his process, to verify that he is moving on the right path towards his goal. The research design includes the selection and presentation of a research problem, formulating a hypothesis, and methodology, data collection, testing of hypothesis, interpretation, presentation and report writing.
Exploratory
Exploratory research studies are also termed ‘formulating research studies’. Exploratory research defines the problem precisely. It is flexible and versatile. It acts as the front end of each research design. The most important principle of the research is to formulate a problem for more accurate investigation (Robson 2008). It also develops the working hypothesis from an operational point of view. The most important in such research is the invention of ideas and insights. This research focuses on the detection of ideas and it is usually based on secondary data. Exploratory research makes use of Surveys of experts, pilot surveys, secondary data collected qualitatively and qualitative research method.
Descriptive
Descriptive research is the one that simply describes something such as demographic, socio-economic, psychographic, characteristics of consumers who use the product. This design is quite different from exploratory research in connection with the purpose and the nature. This research design descriptive research design makes use of the cross sectional design that is collecting data on few factors (Robson 2008). This study is typically concerned with determining frequency with which something occurs or how two variables vary together. This is a pre-planned and a structured design. It works on a prior hypothesis. When the purpose of the research describes the characteristic of the certain groups, the descriptive method is used to estimate the proportion of people with the peculiar behaviour, make predictions in specific area and to determine the associated variables. This research design is mainly used to describe characteristics of market or functions of market customer attributes. Descriptive design makes use of secondary data collected quantitatively, survey, panels, and observations.
Methodology used
This thesis study mainly aims at demonstrating the use of pharmacist, in prescribing medications and treating patients in a primary care setting. The methodology used in this study is a Randomized controlled trials. The study will be carried out at the Highcliffe Medical Centre. The information for this review was provided by the Highcliffe Medical Centre Synergy clinical computer system which produced anonymous reports on the pharmacist led hypertension sessions. 100 hypertensive patients will be taken as control, and they will be treated by Medical Centre’s medical prescribers and another 100 hypertensive patients will be taken as cases and are treated in the pharmacist-led clinic. At the end of the study period, both the study groups are compared for the efficacy in the treatment of the patients by the pharmacist-led clinic in obtaining the desired blood pressure targets.
Patient records were investigated to identify medication prescribed and ascertain blood pressure levels to assess effect of antihypertensive treatment. A questionnaire will be created for obtaining the required data’s for the analysis. To facilitate the analysis of the statistics obtained, the data received from all the groups are tabulated. Matching is done to prevent any bias. Patients who were managed by the medical prescribers, doctors, at the Medical Centre were selected from the clinical system Quality Outcomes Framework database, initially on the basis of matched age and gender to those seen in the pharmacist-led clinic. To prevent any further bias, the 100 patients will be divided into three groups based on raised blood pressure, heart disease and kidney disease. These three groups are then matched among the two study groups. After initial selection patient’s medication records were examined to ensure that cardiovascular, diabetic and renal history matched as closely as possible within the database.
After the tabulation of the obtained data, they are analyzed using the SSPS statistical analysis tool. The statistical dependence can be assessed using the Chi squared test and the Odds ratio. This test is used to compare test statistics representing the frequency of occurrence of a categorical variable, in this case achievement of BP5 blood pressure target. From these the p-value can be calculated, which will help to verify whether the hypothesis of this study is statistically significant or not.
Advantages of this methodology
In this study there is comparison between the treatment by medical prescribers, doctors, at the Medical Centre and treatment by pharmacist-led clinic. In using the Randomized controlled trials as the methodology, the effectiveness and efficacy of the health services provided by the two groups could be assessed. The main advantage is that, the data’s for the study can be easily obtained from the Highcliffe Medical Centre Synergy clinical computer system and the questionnaire distributed among the patients. Since the prevalence of hypertension is high, the cases and the controls used in the study can be easily obtained.
The biases can be avoided by proper matching of the cases and controls. The controls and the cases may differ in age, gender, occupation, etc, which can cause errors in the outcome. This can be prevented by proper comparability between the cases and the controls. Matching is defined as the selection of cases and controls which have selected variables such as age, gender etc in common.
Another advantage is the easier analysis of the data. The final outcome will be in terms of either positive or negative result. The incidence of result, either positive or negative is then tested for statistical significance.
Randomized controlled trials were used in South East London for the evaluation of the efficacy of multi-phased screening trials, which led to the abolition of such screening as they cause wastage of resources.
Disadvantage of this methodology
Although experimental studies are mandatory in the field of delivery of health services, the ethical and logistical considerations often prevent the application of this methodology in the studies concerning humans.
Biases are the main disadvantages of Randomized controlled trials. Matching and randomization can prevent bias to a certain extent, but cannot eliminate it completely. The biases are mainly due to errors of assessment by the human element. This can be prevented by Blinding, which is not done in this study.
Sources of the Information
The information for this review was provided by the Highcliffe Medical Centre Synergy clinical computer system which produced anonymous reports on the pharmacist led hypertension sessions. Patient records were investigated to identify medication prescribed and ascertain blood pressure levels to assess effect of antihypertensive treatment.
Selection criteria and setting
Due to the possibility of interference from other conditions or complications patients will be matched among the three groups as accurately as possible within the Medical Centre patient list.
Influencing factors have been identified as having hypertension at an abnormally young age (less than 40 years of age), raised blood pressure, kidney disease as shown by abnormal renal function tests or proteinuria, ischaemic heart disease including heart failure and, left ventricular hypertrophy or cerebral vascular disease including stroke and transient ischaemic attack (Schroeder, Trehearne, & Ward 2000). Patients will be excluded from the study if they are under 40 years of age, have left the Medical Centre patient list before the end of the study period or had hypertension medication changed by prescribing models not studied, which in this study would be by secondary care prescribers.
Data Analysis and Interpretation
The result of this study will have both qualitative as well as quantitative data. The data’s obtained from the three groups in both the study groups are then entered into a tabular column before doing the statistical analysis. The two matched groups of 100 prescribing patients, one seen in the pharmacist-led clinic, the other by the Medical Centre’s medical prescribers, will be compared for patient blood pressure targets achieved, number of patients lost to follow-up, excluded from treatment targets and whether the medication prescribed was according to national guidance.
To gain a less structured assessment of the patients’ experience of the different blood pressure monitoring services the free text responses will be analyzed to support the quantitative analysis of Likert Scale findings. It is anticipated that by utilizing text analysis on the accumulated responses from each monitoring group to each question that any differences among patient groups can be revealed. To gain a greater depth to the free text responses a hermeneutic approach will be utilized.
The questionnaire based on Likert’s scale and Key Results
Highcliffe Medical Centre
Questionnaire for Blood Pressure Monitoring 2010
Dear Patient,
We would be grateful if you would fill up this questionnaire about your visits for the monitoring of your blood pressure. The feedback received by way of your answers to the questionnaire shall be compared to the approval of patients pertaining to the existing alternatives. This will help us in developing our prospective services. Mr. Howard Lacey, a practicing Pharmacist, is managing this survey and the results will be included in his research for a project to be completed under Doctor of Pharmacy Practice.
The following questions to be answered. There are no confusing questions and it is not indented to reveal your identity.
Thank you.
Please tick or cross your option clearly.
Anonymous details about you to help us categorise your answers.
Are you…….
- Male □
- Female □
How old are you? ________________________
Questions pertaining to the blood pressure service:
- Was your blood pressure been measured by ……?
Please rate your experience at the Highcliffe Medical Centre today by marking one box on each line.
- Was your appointment on a day and the time of your convenience?_____________________________________________ ___________________________________________________________________________________________
If you answered No to question 4 please suggest a more appropriate day and time of day for your blood pressure monitoring.
- Length of time spent in waiting to be seen □ □ □ □ □ □
Please briefly comment on your answer to Q5 _________________________________________________________________
- Making you feel at ease…. (Treating you with respect, being friendly and warm towards you) □ □ □ □ □ □
Please briefly comment on your answer to Q6. ________________________________________________________________
- Letting you discuss any factors you feel may influence your blood pressure reading (letting you tell “your” story)
□ □ □ □ □ □
Please briefly comment on your answer to Q7._____________________________________________________________
- Satisfaction with blood pressure measurement appointment
□ □ □ □ □ □
Please briefly comment on your answer to Q8.______________________________________________________________
- Did your blood pressure medication need to be changed?
Yes □ please go to question 10
No □ please go to question 15
- If you were seen by a Nurse or HCA did you also see a doctor?
Yes □
No □
- How well your medication concerns were listened to?
□ □ □ □ □ □
Please briefly comment on your answer to Q11.___________________________________________________________
- Encouragements to help to you take control of your blood pressure (offered advice on healthy lifestyle alternatives to increasing medication)
□ □ □ □ □ □
Please briefly comment on your answer to Q12.____________________________________________________________
- How well do you think you were involved in the choice of additional medication?
□ □ □ □ □ □
Please briefly comment on your answer to Q13.____________________________________________________________
- Satisfaction with prescribing new blood pressure medication:
□ □ □ □ □ □
Please briefly comment on your answer to Q14._____________________________________________________________
- How satisfied were you with the plan for continued monitoring of your blood pressure?
□ □ □ □ □ □
Please briefly comment on your answer to Q15._____________________________________________________________
- How likely are you to recommend Doctor / Nurse / HCA / Pharmacist blood pressure monitoring to a new patient to the Highcliffe Medical Centre?
□ □ □ □ □
Please briefly comment on your answer to Q16.____________________________________________________________
- How likely are you to recommend Doctor (seen face to face) / Doctor (seen indirectly) / Pharmacist prescribing to treat raised blood pressure?
Doctor seen face to face:
□ □ □ □ □
Doctor seen indirectly:
□ □ □ □ □
Prescribing pharmacist clinic:
□ □ □ □ □
Please briefly comment on your answer to Q17.________________________________________________________________
Thank you, for your participation in this study which will be used to help the Highcliffe Medical Centre to review blood pressure monitoring and treatment services.
Community Pharmacy Practice in the UK
In the UK, there are two types of community pharmacy services. The first one is commissioned by the Department of Health (National Health Services) and comes under NHS Contractual Framework. The second one falls outside the scope of the NHS contractual framework. The scope of the NHS contractual Framework is much wider than non-contractual pharmacy services offered.
NHS Community Pharmacy Contractual Framework
This is a tri-party agreed framework for delivering pharmacy services in the United Kingdom under the department of health. The first such frame came into existence in April 2005 in line with the vision set out in July 2003. The collaboration is agreed and supported by the Department of Health (DH), NHS employees (NHS Confederation) and PSNC (Pharmaceutical Cervices Negotiation Committee) (Department of Health-UK 2005). This framework is mainly drawn open the utilization of community pharmacy’s skills, experience and expertise of pharmacists and staff. The community pharmacy is considered an integral part of health care and is expected to support patients in self-care, respond to varied needs of communities while remaining innovative to tackle health inequalities. Under this framework, there are three categories or levels of services. These categories are essential, advanced and enhanced community pharmacy services (see figure below).
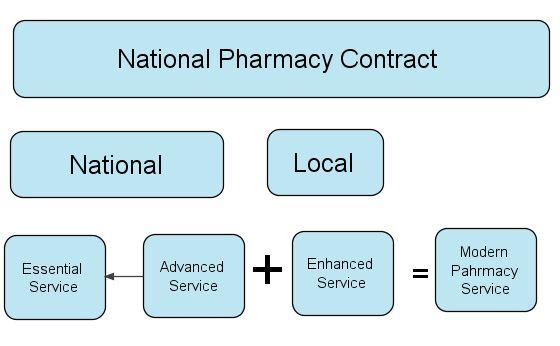
There have been certain changes to old framework under the Pharmaceutical Services (Advanced and Enhanced Services) (England) Directions 2011 (Department of Health, 2011). Major changes made are the introduction of New Medicine Service for people with long term conditions, introduction of national target group for MUR and changes in clinical governance to strengthen existing clinical governance in community pharmacy.
Future provision for contractual pharmacy up gradation is clearly addressed in the new contract framework. The services which are advanced and enhanced category services can be moved onto the next level i.e., essential services. There is scope to include more services under advanced and enhanced service categories in future.
Essential Services
Essential services are services every community pharmacy contractor should offer to the community under contractual framework. This is the minimal level of service under the framework. The dispensing and repeat dispensing is the primary responsibility along with public health promotion, electronic transmission of prescription, sign-posting to other health professionals and services, disposal of unwanted medicine, providing support for self care and clinical governance. In 2005, the NHS Community Pharmacy contract came into existence. According to this contract, pharmacies throughout the country were obliged to render the following services to their customers:
- The pharmacy has to strictly follow the prescription and label the medicines as per the instructions of a General Practitioner or other certified and approved healthcare provider who is authorised to prescribe medicines. Apart from a doctor, such a person can either be a nurse, a dentist or a pharmacist.
- If any patient needs to get medicines frequently, over a period of time, he/she can request his/her General Practitioner for an authorization to get the medicines for that particular period. It means that if the authorization is made, then every time the patient needs medicines, he/she doesn’t have to visit the General Practitioner. He/she can straight away go to the pharmacy in his/her locality and get the medicines.
- If any patient feels that he/she is totally cured and doesn’t need medication anymore and if there are certain medicines that have not been consumed, he/she can visit the pharmacy from where the medicines were taken and can return them so that the pharmacy may be able to dispose them safely.
- Healthy lifestyles are promoted under this service. Such healthy lifestyles include quitting smoking, healthy eating habits, following a daily exercise routine and other such habits that may have an impact on the people’s health. Pamphlets and other material are distributed among the people for general awareness about their health. Promotional drives are organized that spread the awareness on various topics such as precautions to be taken while out in the sun, etc., and also about the threats involved in prolonging fatal diseases like diabetes, etc.
- The Pharmacy is supposed to provide information on any other medical related services to its customers.
- The pharmacy is supposed to provide information on precautions to be taken in order to avoid common diseases like cough, cold, nausea, etc., and their treatment.
Advanced Services
Advanced Services are opt-in services provided by community pharmacies under CPCF (Community Pharmacy Contractual Framework). These are service in which a pharmacist and/or premises used to provide service are to be accredited by authorities to provide such services. Advanced Services include Medical Use Review (MUR) Service, New Medicine Service (NMS), Appliances Use Review (AUR) Service and Stoma Appliances Customisation (SAC) Service.
The MUR (Medicine Use Review) is the first advanced Service introduced in NHS in which medicine use review is conducted by accredited pharmacist in accredited premises to maximise effective use of medicine and reduce medicine waste. The main focus of the review is adherence to the prescribed and non-prescribed medicine use and any changes to be made in the way prescribed medicines are being used for long term conditions. It is aimed at helping patient to understand their therapy and enable them to make changes to medicine use according to their needs and problems faced in using medicine. The MUR should be conducted face to face in normal circumstances. Telephonic mode can only be followed where it is not practically possible for face-to-face MUR. This should be conducted only after permission from PCT. There should be a designated area for MUR session, essentially separated from common public area of pharmacy. Three target groups should consist at least fifty percent of all MURs. These target groups include patients taking high risk medicines, patients recently discharged from the hospital and patients prescribed certain respiratory medicines.
The second advanced service is Appliances Use Review in which patient experience of appliance use is reviewed, understood and if any, changes to appliance use are made to enhance the benefits of such appliances use. The Stoma Appliances Customisation as per the patient’s measurements done by pharmacist under contract is third service under the contract.
New Medicine Service is recently added in the contract framework (PSNC, 2011). This service provides support to patient with newly prescribed with a medicine to help in effective use and patient adherence of the medicine. The service is for initial period of two years and may be extended for additional period if all parties agree. There are three stages of the service. First stage is patient engagement. The patient can be recruited by prescriber or by pharmacist. The initial disease included for the services are asthma, COPD, Type two Diabetes Mellitus, anti-platelet and anticoagulant therapy and hypertension. In the intervention stage, the adherence to medicine will be assessed and help will be provided including any change or interventions necessary.
Enhanced Services
The most modern service of the included in contract is Enhanced Service, which is specifically designed to meet local needs in a Primary Care Trust (PCT) and is provided by PCT. These services are commissioned and funded by PCT. Some of the examples of such services are care home service, specific therapy service, school service, stop smoking service and home delivery service. Supplementary and independent prescribing also form an important part of this service which allows community pharmacists to practice as an independent prescriber in some case and supplementary prescriber. Moreover, pharmacist can provide out-of-hour and minor ailment service under this category.
Power and Authority in Pharmacy Contract
New pharmacy contract is directed by grid lines issued under Pharmacy Services (Advanced and Enhanced) Directions 2011. Directions address the issue of authority and rights under the contract along with responsibilities of contractors. These directions are issued under Health Service Act 2006. The contractor pharmacy service provider should be responsible for fulfilling certification requirements for providing advanced and enhanced service in premises appropriate as detailed in the contract. The PCT is responsible to make arrangements for advanced and enhanced services under the act. The contractor pharmacy is also responsible for record keeping, record providing and sharing the practice information with other care providers as and when required with greater responsibility to protect the patients information in manner deemed to be in line with the protection of the privacy and confidentiality in the patient data.
Benefits of New Contractual Framework
There are multiple benefits expected from introduction of the new community pharmacy contract framework (PSNC, 2011). It is expected that they will save in GP time. Expected eighty percent of repeat prescriptions will be handled by community pharmacies to save 2.7 million hours of GP time. It will further reduce burden of work for GPs and save money on long run. The framework is aimed at increase the availability of the service in wider range and increase the QoF (Quality Outcome Framework) for long term conditions like asthma, diabetes mellitus and hypertension. From new contract, it can be implied that the payment will include the quality of service along with the amount of work done.
Non-Contractual Pharmacy Services in UK
Non-contractual independent pharmacy practices make only a small part of pharmacy sector in UK. The major proportion of services provided out of the contract are related to travel medicine, vaccinations not covered under NHS, life style medications like medications for erectile dysfunction and weight control with certain medications not approved under NHS. The proportion of out of the contract revenue for community pharmacy is limited and only account for nearly one percent of total revenue as much of revenue come from NHS Pharmaceutical Contract services detailed in previous section.
The provision of dispensing over the counter and prescription only medicine for travel purpose is to help international travellers to cope with expected and unexpected health threats during and after the travel schedule. One of the services can be and often offered by community pharmacist is travel vaccination. Hess (2010) examined the acceptance rate of travel vaccination services by pharmacists in which they observed that acceptance ranged from 97% (yellow fever) to sixty seven percent for polio with an average of 87%. Gatewood et al (2003) concludes that a comprehensive travel health package in a super-market is successful and provide alternative to traditional health access. Hind et al (2008) examines travellers’ preparedness to make a payment for travel medicine check-up and vaccinations and acceptance of the service from a community pharmacy. They conclude that the people are ready to be helped before travel by community pharmacists and are ready to pay for the same.
As per the reports of National Pharmacy Association, 5-20 % of UK men have erectile dysfunction. NPA support, train and help community pharmacists to deliver const effective erectile dysfunction service in communities. The service is aimed at increasing need on the community pharmacy services which are not part of NHS coverage. Clinical pharmacists are even employed by many HIV and sexual health specialist clinics in NHS itself; the independent prescribing on private basis is also gaining popularity. The service provided for this sensitive health issue will further get support and acceptance from service users as well.
Similar to travel health services and erectile services, the weight control services are also in use from pharmacist led clinics where service user access service nearest to their work place or residence. The services are delivered on the needs and demand in the local community to help individuals remain fit and act proactive towards preventive health measures.
Portfolio Working in UK Pharmacy Profession
A pharmacists and a pharmacy technician can work in a hospital pharmacy, in a community pharmacy, in primary care, in a prison health facility or in armed forces. Along with these roles, recently there is increasing trend of working as a locum pharmacist, where the pharmacist work as a relive worker or freelancer when there is short to medium term needs arise. Many of pharmacist work as locum because of the formalities and papers work involved in full time basis work but there many others who find it difficult to work full time like females who have children or are planning for the same or many other engagements in their personal and professional lives to meet the requirements (Shan and Hassel, 2006). Many of pharmacists opt for a locum pattern to make a work-life balance.
Noticeable patterns found in study conducted by Shan and Hassel (2006) are hospital plus retail, retail plus primary care, community plus primary care, hospital and primary care and so on. There have been some pharmacists who work on full time basis but work on locum basis on weekend or during holidays. The locum during holidays and weekend along with a full time pharmacy job is supposed to be because of additional financial responsibility or drive to earn more. The study also commented on the respondents’ remarks about why they chose to be locum and state as to how the amount of work relieves the stress, as working as locum have lesser paper work, responsibility and stress related to the work along with great satisfaction by helping patients to remain healthy. The so called portfolio work is adapted by pharmacists to enhance their knowledge and experience as one of the respondents cited the reason to work in community pharmacy. He thought that the one who only works for a hospital or primary pharmacy job will not have the knowledge and experience about what it meant when a patient is encountered in community.
The portfolio working and part time working is also one of preferred working pattern opted by female pharmacists. These pharmacists have other responsibilities of raising children and work as home makers and have a fraction of the day available to work as pharmacist. The options available are those in community and hospital. Community female pharmacists working on part time basis usually work flexibly to make balance in personal and professional obligations.
As a pharmacist, I have observed varied choices opted by pharmacists. Most of the pharmacists opt or work for only one type of pharmacy facility. However, many of the pharmacists prefer to work for a couple of roles within pharmacy profession. This portfolio working in case may involve working as a retail or hospital pharmacists besides being an independent prescriber in community clinics led by pharmacists, or as a health care or self care support work along with community pharmacy portfolio.
DEPEST Analysis of Community Pharmacy
In recognition of the need for change in an industry it is important to consider the strategic position of the industry whether it is in decline or growth, compared to the wider market. Other factors which will influence the need for change consist of changes to the legal framework and social environment in which the pharmacy industry operates. The DEPEST analysis tool has been developed to assist with strategic business planning by allowing a macro-environmental assessment of trading to be examined. PEST analysis takes into consideration the Demographic, Epidemiological, Political, Economic, Social and Technological influences on the industry.
Demographics of the population registered under the practice are given in Appendix C. The current population registered under the practice is 9903 (4639 male and 5264 female) out of which 55% are above the age of sixty years. Moreover, there are around 18 percent of population consisted of those who are above the eighty years of age. Current practice population is lower as compared to that in 2008. The decrease in registered population with practice might be because movement of people or changing demographics.
Epidemiologically, the high blood pressure is the one of very common conditions in world and in England as well. The blood pressure of ≥140 mmHg systolic and ≥90 mmHg diastolic is classified as high. When considering the prevalence of hypertension in England it may vary a bit from community to community. In England, about 33 % male and 25% females in age group 45-54 are hypertensive. Hypertension increases with age and above the age of 75 years, 73% of men and 64% of women are hypertensive. Although the prevalence rate in practice is not clear but if it is considered almost similar to that in England, the rate can be labelled as high. This high prevalence requires resources to address the need for the change in current practices of GPs monitoring and managing high blood pressure.
The political factors for most industries are restricted to legal changes, taxation and tariffs set by the government, but in the case of pharmacy the government influence extends into the economic factors. Legal framework support mainly community pharmacy practices. There are many pressure groups opposing introduction of NMS service and other advanced pharmacy services. These pressure groups are also voicing their opinion negatively for enhanced pharmacy services. The impact of such lobbying may slow down the progress in independent prescribing by pharmacist. Many of such groups call prescribing and supplementary prescribing practitioners as ‘quacktitioners.’
Economical factors play important role in any industry. Main source of income and profit is payment under NHS contract. Only less than 10% income is generated from non-contractual services which also includes OTC sales and practising as an independent prescriber or as a travel health reviewer. Increasing market share of supermarket retailers and parallel imports of medicine poses another threat to community pharmacy practices.
The Social factors represent changing customer and trade behavioural trends. Increasing purchasing from supermarket offer convenience and cost cutting on various OTC medicines and other allied healthcare products may reduce future sale from a community pharmacy.
Increasing use of technology in record keeping, dispensing and information collection and transmission offers innovations they way medications and health care is delivered. Electronic Prescription Services are being used in dispensing where prescriptions are directly transmitted to a community pharmacy where the patient is registered. There are possibilities of using robotic dispensing services in future to reduce human interface in the dispensing process. The technology in one may reduce the manual workload but on other hand may reduce demands for trained pharmacists and pharmacy technicians.
Discussion
Pharmacist as an independent prescriber is a new concept introduced in medical practice. The outcomes of hypertension clinics conducted by pharmacists are encouraging in both ways. The pharmacy practice at the medical centre is part of newer independent prescribing roles pharmacists are playing in other parts of country and in the world on larger scale. Initial results of the study suggest that the independent prescribing by pharmacists and other health care providers, other than doctors will bring changes in the way of improving health of a population. The future of independent prescribing role of the pharmacist is expected to get support from all sectors as it is delivering result comparable to doctor led prescribing. However, the training, continued professional development, and long term support for pharmacist working as an independent prescriber are necessary. During the years, there have been some very encouraging and important developments pertaining to pharmacy. Perhaps the most important of such developments has been the amendment in the law that now allows pharmacists to write prescriptions. This has helped the patients and has also reduced the work load of doctors and other prescribing authorities. This way, the pharmacists can have better and greater interactions with the General Practitioners and their customers. There is a term called ‘Pharmacists with a Special Interest (PhwSI) which means such pharmacists who have expertise in treating certain ailments like arthritis, etc. Since PhwSis are experts in the treatment of some particular ailment, they can provide better services and results to patients having those ailments.
The future of community pharmacies is full of opportunities for the pharmacies and better treatments for the patients. The amendments in the law have provided an added advantage. The growing number of community pharmacies throughout the country has made access to such pharmacies very easy.
Pharmacy Profession and Independent Prescribing
It has been observed from historical evidences that the pharmacy profession was an integral part of healthcare delivery in early stages of medical sciences. The composing, formulating dispensing roles were played by single individual in earlier medical practice. The evolution of pharmacy as a separate profession came in view after advancement in medical and surgical specialities where numbers of medicine in use increased and methods of formulation, packaging and dispensing advanced. The packaging and formulation of modern medicine advanced alongside the new knowledge in the area of administration of medicine into body. Routes other than oral route gained popularity and use of injection led to the development of parental administration of medicines and drug preparation to bypass gastrointestinal process of absorption and processing of medicine before these can be effective at the site of requirement in the body. Still the development of oral medical formulations has major proportion of medicine administration as it does not require professional help to take medication. However, the specialized knowledge of a disease process and medicine is pivotal to get better outcomes in the terms of relieve from sufferings because of an ailment. This knowledge is possessed in part by many professionals. The pharmacist had in-depth knowledge of medicine formulations and their side effects. They are also equipped with modern day knowledge of disease processes and pathologies associated with diseases.
Independent prescribing by pharmacists and other healthcare professionals is helping healthcare providers and policy makers to make maximum utilization of varied knowledge base and workforce. The workload of medical practitioners and doctors is increasing day by day and cost of services provided by doctors are higher as compared to the cost of services provided by allied health professionals like pharmacists, nurses, podiatrists and physiotherapist. Comparatively lower costs and increased access of healthcare is aim of all policy making agencies. The access to health care can be increased in two ways. One is increases the availability of doctors especially general practitioners to meet increasing demand on healthcare resources. Secondly, it can be achieved by maximizing the use of skills and knowledge possessed by other healthcare professionals.
When it comes to medication review and advice on a disease which needs administration and use of medicine preparations, the pharmacists’ expertise is of outmost importance. The specific understanding of all aspects of medication being used in a particular condition put pharmacists ahead of other healthcare providing professionals.
The prevalence of the hypertension varies and increases as the age bracket progresses from young age to over eighty years of age. The overall, around 12 % of UK population is suffering from hypertension, which makes it one of disease causing extensive burden on healthcare services. The use of clinicians instead of a doctor will save the doctor time as well as money. It is expected to increase the access to healthcare in general. By re-channelling patients from traditional doctor led clinics to pharmacists led clinic will save GP time which can be utilised to address other healthcare needs of community.
The Highcliffe Medical Centre Results
The outcomes of pharmacist operated hypertensive clinics are comparable to nurse provided service and are better than health care assistant provided help to control the high blood pressure. As it is obvious from the study that Quality outcome frame work results were favourable in prescriber pharmacist conducted hypertension clinics, it is in-fact helping NHS to meet quality targets set to achieve better health. The pharmacists are in better position when the supplementary prescribing is considered. There are strong arguments in support. The knowledge of a pharmacist is much deeper about the drug regimens and their properties. The pharmacists are equipped with skills of managing medicine regimen very well.
Drugs acting on angiotensin-renin system were most frequently prescribed medication as compared to thiazide diuretics and beta-blocking agent. These drugs are most preferred medicines in pharmacist led hypertensive clinic as the dosages can be started from lowest can be increased to optimise the pressure control. These medications are also known for lower and less severe side effects. Commonest side effect noted is cough and is experienced by ten to twenty percent of users. Calcium channel blockers were less frequently prescribed caused more side effects. The acceptability for the same reason was lower for this group of medications as compared to beta-blockers and diuretics. Well established uses of the diuretics and beta-blockers promise pressure control but are not free from unwanted side effects and forms less preferred medications by patients.
At the medical centre, pharmacist led clinics were held to treat patients referred by nurses or healthcare assistants to recheck the blood pressure noticed to be high in nurse room or at healthcare assistants blood pressure screening clinic. The choice of the preferred and effective medication depends on the age group of the patient and the side effects of the medicine in use. Many patient groups may have ongoing treatment for other co-morbid conditions which need other medicines to be used. The choice medicine is not easy and may need referral to General Practitioner doctor for further evaluation for the suitability of the medicine but later on the medicine use review can be carried out once again by pharmacists alone to monitor the efficacy of medicine and adherence by the patient. The results of medicine prescribed in pharmacy clinics are encouraging. Majority of patient achieved their target blood pressure after first prescription in the clinic. The most of rest achieved it on increase in the dose of the prescription medication or with help of additional medication.
The monitoring of blood pressure at patient’s will is more important. Many of respondents would prefer to be seen in morning hour or on weekends. The reason for this preference is can be convenience of attending the clinic. They want to attend when they have time available. The waiting time in a clinic also affect patient choice about the clinic or professional. This wait was less in pharmacist clinics. In many parameters, the satisfaction level in pharmacist-led clinic was better as compared to HCAs and was comparable or better as compared to nurse clinics.
This satisfaction level is also reported in other studies discussed in literature review and results analysis. Even international studies support that pharmacist-led clinics are cost effective as compared to physician clinics and are also in operational state in other countries.
The role of pharmacist in community pharmacy and community health care is gaining more acceptances from communities and from authorities and policy makers. There two main reasons for the same. First one is to improve the access to health care by diverting more patients to pharmacist clinics. This eventually saves physician time. The second one is cost factor. The cost of a pharmacist clinic is less than that of a physician led service.
Training and Career Development for Pharmacist
The pharmacist can provide services other than hypertension service. These ranges of services are part of advanced and enhanced services category of the contractual framework. The service in which pharmacists can be of much use, are long term conditions like diabetes, life style diseases, weight control, community services in heart disease awareness, and services related to sexual health. As pharmacists posses required knowledge about various medications, their future role can focus on the medication and review of medications in various health conditions. Skills to deal with patient counselling, advice, and guidance on life style require different set of skilfulness. The skills including soft skills can be enhanced by having an integrated training and development plan for individual pharmacists.
The additional training specific to the dealing with consultation, counselling, dietary advice and lifestyle change can be provided in structured manner to enhance pharmacist’s ability to manage hypertension in community clinics.
The training requirements as and when required should be structures on the basis of previous skills and knowledge possessed by pharmacists. Apex bodies related to profession in collaboration with other healthcare agencies can have mentoring programmes covering all aspects of supplementary and independent prescribing. Professional body for pharmacist can be involved in training and professional development. Training can be provided in community setting to maximise keep the training practical rather than putting emphasis on the theoretical aspects.
Future of Independent Prescribing
The role of pharmacist and independent pharmacist prescriber is still in evolving phase. Pharmacists too are taking different roles and switching their stand from a dispenser to a healthcare professional providing patient care. Policy makers and healthcare authorities are formulating policies for modern healthcare services with increasing representation to pharmacists. The services delivered at door steps of users are gaining importance and pharmacists are nearest of all care providers who are skilled and authorised to provide medications and care of long standing medical and surgical conditions with need of continuous care.
With the provision of introducing newer advanced and enhanced services under new pharmacy contract, the role of pharmacist takes different but stronger foot hold in providing community health services. There is also a future plan to move some or all of the advanced and enhanced services to essential category. If this happens in near future the workload and care responsibilities of pharmacists will be equal to that of a nurse or a doctor in community practice.
Hypertension – Key Facts
Hypertension is the persistent elevation of blood pressure above normal values and it is a common disease condition that affects between ten and thirty percent of the population of the United Kingdom with the prevalence increasing as the population ages (William et al. 2004). Hypertension is usually defined as transitory or a sustained increase in the systemic arterial blood pressure to a level likely to induce cardiovascular damage or other adverse consequences. The normal level for blood pressure for an individual is below 120/80, where 120 represent the systolic measurement (peak pressure in the arteries) and 80 represents the diastolic measurement (minimum pressure in the arteries). Blood pressure level between 120/80 and 139/89 is termed as pre-hypertension (to denote increased risk of hypertension), and a blood pressure of 140/90 or above (i.e., above 140 mmHg systolic pressure and 90 mmHg diastolic pressure) is internationally recognized as hypertension (WHO/ISH Writing Group, 2003 4 /id). In Western Europe it is believed that nearly one third of the population suffer from hypertension and as it is a symptom less condition which represents a major risk factor for cardiovascular and renal disease it also known as a ‘silent killer’ (Primatesta et al. 2001).
In most cases, the cause of hypertension is never known and the condition is described as essential hypertension. In some cases, the basis of the disease is established and such cases are said to be secondary hypertension. Hypertension increases with increasing age till 90 years of age, after which there is a slight reduction in incidence compared to the previous decade (Casigia and Palatini 1998). It is believed that the increased incidence of hypertension in the older population is due to an age-related increase in arterial stiffness (Safar 2005). The patients reviewed in the pharmacist prescribing clinic are mainly those who were suffering from essential hypertension although many may have developed hypertension due to age-related loss of vascular elasticity.
NICE Guideline on Hypertension: The guidelines followed by NICE were revised due to the fact that fresh information about the treatment of hypertensive patients was received through the data from clinical trials (NICE Clinical Guideline 2004). Hence, the concern was limited to the suggestions on the pharmacological management of patients with hypertension as is mentioned in the fourth part of the first chapter of NICE guideline. Some of the guiding principles were not reviewed and remain to be considered as the latest ones. The National Collaborating Centre for Chronic Conditions assumed the task of working on the guidelines. The Centre is located in the premises of the Royal College of Physicians of London. The twin aims of the centre are to include new facts and figures in the guideline and to corroborate with the British Hypertension Society (BHS) in order to formulate new procedures to be followed by primary care prescribers at the NHS.
Dietary Approaches to Stop Hypertension (DASH): What you choose to eat affects your chances of developing high blood pressure, or hypertension (the medical term). Current studies prove that the Dietary Approaches to Stop Hypertension (DASH) can be useful in lowering the blood pressure. Consuming less salt (Sodium Chloride) can also be helpful in reducing the blood pressure. Although both the steps are individually useful in reducing the blood pressure, yet if both are followed simultaneously, situations of having high blood pressure can be avoided. The relation between the salt ingestion and blood pressure is that lesser the salt ingestion, lower will be the blood pressure. According to results based on studies, DASH menus with 2.3 grams of Sodium have the tendency of lowering the blood pressure and those with 1.5 grams of Sodium can additionally lower the blood pressure. These menus have lower Sodium contents than the average sodium ingestion (per day) by adults in the United States of America; 4.2 grams by males and 3.3 grams by females. People suffering from high blood pressure or hypertension can benefit a lot by pursuing the Dash menu. The normal blood pressure level is 120/80 mmHg, and it can be harmful for a person to have even a little higher level. As the blood pressure level rises, so does the risk. According to studies carried out by scientists of the National Heart, Lung, and Blood Institute, blood pressure could be controlled or reduced by following a healthy eating plan constituting of low cholesterol and fats. Emphasis was laid on fruits, vegetables, low fat milk and its products, grains, fish, poultry products and nuts. The mentioned food products have greater percentage of all necessary minerals, proteins and vitamins. The same ingredients are approved by the Institute of Medicine.
An initial DASH study was conducted with 459 patients. The blood pressure of these patients was in the range of 160 to 80-95 mmHg. Out of these people, fifty percent were men and sixty percent were African immigrants in America. Also, twenty seven percent suffered from high blood pressure. These people were asked to randomly follow one of the following eating plans: eating plan of a normal American, extra fruits and vegetables in addition to the eating plan of a normal American, and the DASH plan. It is noteworthy that all the eating plans were non-vegetarian and had a daily ingestion of 3.0 grams of sodium. The results started showing changes within two weeks of starting the eating plans and witnessed reduced blood pressure in people who followed the eating plan with extra fruits and vegetables and also in those who followed the DASH plan. Out of these two plans, the DASH plan was more effective in reducing the blood pressure.
A second DASH study was conducted involving 412 people and they were asked to randomly follow either the DASH eating plan or the eating plan of a normal American. One change that was made in the diet plans was that the sodium intake was reduced. This was done in three stages (one month for each stage). The first stage required participants to ingest 3.3 grams of sodium daily (equivalent to the sodium ingested by a normal American on a daily basis), the second stage had 2.3 grams of sodium ingestion and the third stage had 1.5 grams of sodium ingestion. A reduction in the blood pressure was noticed in each stage, as the sodium content was reduced and as such, the lowest blood pressure level was noticed when people followed the eating plan with 1.5 grams of sodium ingestion per day. People suffering from high blood pressure or hypertension were benefitted the most. So it is advised to follow a DASH eating plan to control the ingestion of sodium.
If you need to lose weight, even a small weight loss will help to lower your risks of developing high blood pressure and other serious health conditions. At the very least, you should not gain weight. A recent study showed that people can lose weight while following the DASH eating plan and lowering their sodium intake. In a study of 810 participants, one-third of them were taught how to lower their sodium intake and follow the DASH eating plan on their own. Most of them needed to lose weight as well. They followed the DASH eating plan at lower calorie levels and they increased their physical activity. Over the course of 18 months, participants lost weight and improved their blood pressure control.
Blood pressure is the pressure with which blood strikes against the walls of the artery. The unit of blood pressure is mmHg i.e., millimetres (mm) of mercury (Hg). It is denoted in twin numbers; the first one is called systolic second one is called diastolic. Systolic pressure is the blood pressure when the heart beats and diastolic pressure is the blood pressure between two heart beats. Both the numbers have their own significance. It is normal for blood pressure to experience increase and decrease during the course of the day but it is a matter of concern if the increase in blood pressure persists. The reason being that due to the high blood pressure, the heart has to exert more and also, the arteries and various organs of the human body are damaged. There are no symptoms for increased blood pressure. But once it is increased, it keeps on posing problems throughout the life. But further increase in blood pressure should be controlled otherwise the person can become a heart patient.
High blood pressure can be avoided by maintaining the weight of the body in proportion the body height. It has been observed that almost 33% of American adults suffer from high blood pressure. Also, African Americans have a greater tendency of having high blood pressure than the whites.
Be moderately physically active on most days of the week, follow a healthy eating plan, which includes foods lower in sodium; if you drink alcoholic beverages, do so in moderation; if you have high blood pressure and are prescribed medication, then you should take it as directed.
Summary of the Hypertension Surgeries
During 2008 there were one thousand one hundred and forty seven appointment slots scheduled although only nine hundred and sixty nine were available for hypertension patient consultations. The difference in these two figures represents the scheduled sessions allocated for routine administration; catch up time and to allow for prescriber breaks during the session.
Over the year there were one hundred and eighty seven appointments that were still available to be booked at the scheduled time representing approximately nineteen percent of the total. Of these unfilled appointments one hundred and seven, or eleven percent of the total appointments, were as the result of cancellation. With the age of the patients being consulted there is an increased risk of cancellation. Cancellations could be due to causes such as, adverse weather conditions or the need to attend hospital appointments hence the high number of cancelled appointments. Four percent of appointments were missed by the patients, classified as did not attend on the clinical system, which in view of the age distribution of the patients is not unsurprising as forgetfulness increases with age (Hanninen and Soininen 1997).
Ten percent, seventy three, of patients arrived after the scheduled start of the appointment time and the average patient waiting time over the year was nine minutes after the scheduled start time. Forty six percent of appointments were started on time or within five minutes of the scheduled start time and forty three percent of appointments ended within the allocated appointment time.
While the vast majority of patients seen in the pharmacist hypertension clinic were registered by the National Health Service with the medical centre two were temporary residents. These temporary residents required the urgent supply or a prescription to allow them to continue treatment prescribed elsewhere but left at home when coming to visit Highcliffe on holiday.
All the patients seen were over the age of sixteen years with seventy nine, ten percent, being aged seventeen to sixty four years and the balancing ninety percent being sixty five years or older. Of the patients referred to the pharmacist hypertension clinic twenty six percent did not need to be seen more than once, indicating that their blood pressure targets had been achieved when seen. This high proportion could be due to patients being more at ease when their blood pressure was recorded in the pharmacist clinic or having increased adherence with previously prescribed antihypertensive medication. The majority had been referred as the result of a raised blood pressure reading taken a few days previously by the medical centre health care assistants.
Approximately forty two percent of patients were twice seen indicating that prescribing changes quickly achieved target blood pressure levels for these patients or that they were previously not regularly taking their antihypertensive medication. Failure to adhere to an agreed treatment plan is common among older patients suffering from asymptomatic conditions like hypertension (Hyre et al. 2007). It is a standard practice to review the effect of prescribing changes one month after the introduction of a new medication or dose change in an existing medication. However, in cases of severe hypertension, review at a shorter interval is necessary and these would normally be treated with a supporting general practitioner.
Sixteen percent of patients were seen three times, a further six percent required four appointments, and seven percent needed to be seen five times. The remaining three percent of patients required either six or seven appointments during the year. The high number of appointments for these last two groups of patients being due in part to a six monthly repeat review of blood pressure or a need to change medication for patients who report adverse reactions to prescribed treatment.
The age distribution of hypertension patients for which new medication was prescribed by the pharmacist approximately reflected the age profile of hypertension patients at the Medical Centre. Ten new prescriptions were issued to patient in their fifties, twenty three in the sixties, sixty five in the seventies, sixty four in the eighties and six to those in their nineties. Fig 1 shows a graphical comparison of patient age for prescriptions issued and ages of patients on the hypertension register.
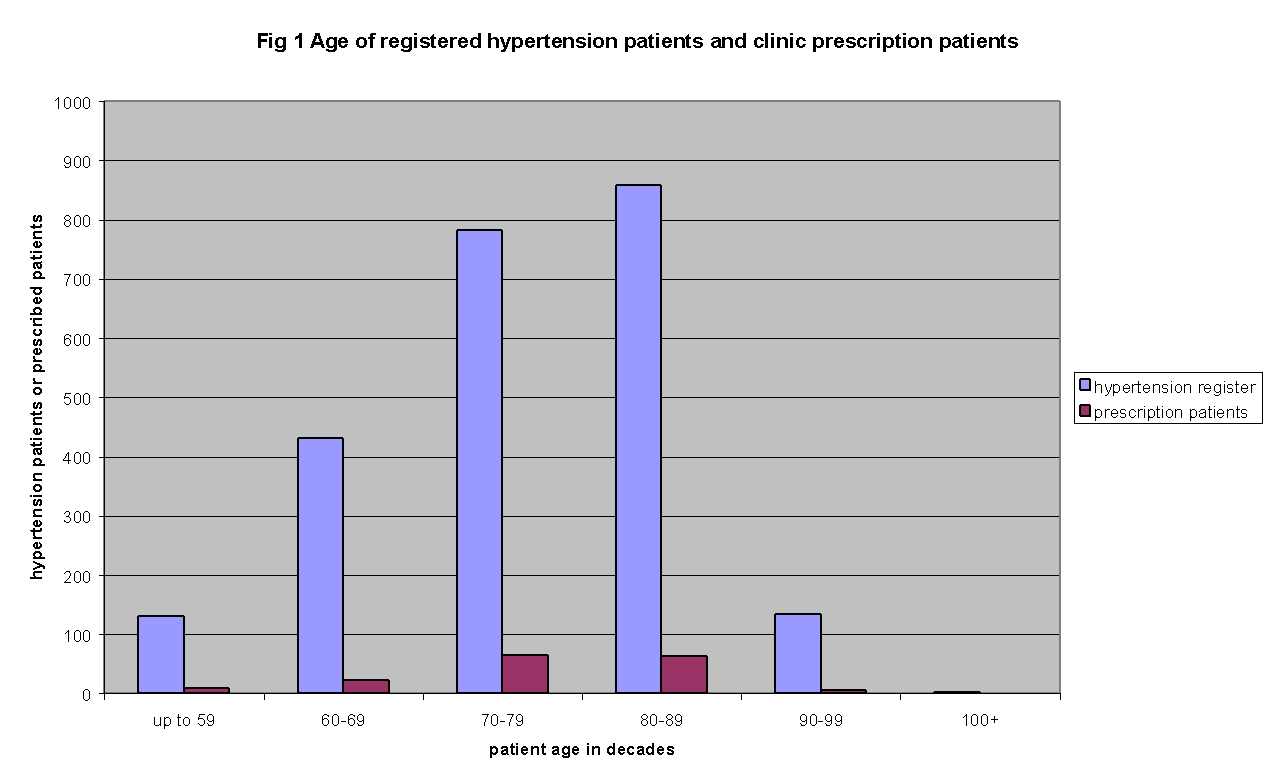
It can be seen from Fig. 1 that the patients prescribed for by the pharmacist-led clinic had a small bias towards younger than average patients. This can be partially explained by the invitation of younger patients to the Saturday workers clinics. Other factors involved in the bias toward younger patients could include the increased difficulty in attending the hypertension clinic in the Medical Centre by older patients and an increased likelihood of patients being recorded as being on maximum tolerated medication. The pharmacist led hypertension clinic did not perform any domiciliary visits during 2008 and it is not currently planned that the service will be extended to the housebound.
Targets for Treatment at the hypertension clinic
Patients were treated in the hypertension clinic to achieve target blood pressure levels recommended by the relevant guidelines and as required by the Medical Centre contract requirements (BMA & NHS Employers 2009). There are different requirements for the management of blood pressure in simple hypertension, in patients with diabetes and in patients with chronic kidney disease (BMA & NHS Employers 2009). The Quality and Outcomes Framework targets are set out in Fig. 2.
Table 2: Medical Centre hypertension targets from QOF
The effect of the Drug Tariff category M pricing of drugs
What are category M drugs?
Category M drugs are the standard medicines that are easily available in the market. The prices of such medicines, obviously controlled by the Department of Health, depend on the feedback from the manufacturing companies regarding the sales volume. These prices are reviewed every three months. The prices are available online as well on the PSNC portal. There are about five hundred standard medicines that come under the category M drugs.
Requirements for drugs to enter the UK market
The United Kingdom Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMEA) are the two governing bodies that authorise drugs/medicines to be marketed in the United Kingdom. The medicines are supposed to be harmless, with minimum side effects, once they get approval from the MHRA or EMEA. There are three categories under which the medicines are authorized. These are Prescription Only Medicines (POM), Pharmacy Medicines (P), and General Sales List (GSL). Some of the medicines under the POM category are allocated as Controlled Drugs (CDs). Such medicines need special care in their usage.
What are the criteria for pricing the medicines?
Pharmaceutical companies generally market a medicine that has been generated by them, under their own brand name. Such medicines are protected by a patent so that no other company is able to manufacture similar medicines until the patent duration expires. Even after the expiry of the patent duration, other companies cannot bring out a medicine with similar name, although the ingredients can be similar. Such medicines are called generic medicines. It is noteworthy that since acquiring a patent for a medicine involves a lot of expenditure, the cost of patent is added to the cost of the medicine. Hence it is understood that a patent medicine will always be costlier than its generic version.
It is obvious that it will be beneficial, monetary wise, if more generic medicines are introduced in the market. Since these medicines are expected to save numerous lives, the United Kingdom government spends a handsome amount on the development of new medicines and their generic versions. It is estimated that “The NHS spends about £11 billion a year on these treatments, £8 billion of which is on branded drugs” (OFT 2007).
The pharmaceutical companies manufacturing patent medicine don’t have a free will to price their patent medicines. The Department of Health has put into effect the Pharmaceutical Price Regulation Scheme (PPRS) by virtue of which the department controls the prices of the medicines.
Functions of the Pharmaceutical Price Regulation Scheme (PPRS)
- Introduce new life saving drugs and drugs that treat critical illnesses, in the market every year.
- Control the expenditure incurred by the Department of Health on branded drugs.
- Control the prices of new drugs being introduced in the market. This is done by controlling the profits earned by the manufacturing companies.
- Control further price increase by the manufacturing companies.
Effects of PPRS policies
It has been observed that in a few cases, the PPRS has not been able to control the high prices of some main medicines. It hasn’t taken into consideration the therapeutic values of the medicines. There are cases where substitutes of medicines have been priced as low as 500% as compared to the patent medicines. This has obviously taken a major share of the allocated budget. If the prices had been contained, the amount could have been used for some constructive and beneficial purposes. “Reviewing some major drug categories on an indicative basis we identified over £500 million of expenditure in 2005 that could have been put to more cost effective uses” (OFT 2007).
The high prices of patent medicines prevent the patients from buying such costly medicines and as such, they cannot benefit from the new medicines that have been introduced.
Due to investment in high priced medicines, the NHS is short on financial resources, and as such, is not able to provide incentives to other pharmaceutical companies that engaged in manufacturing life saving drugs.
What requires to be done?
The following action could be taken in order to resolve the problem faced by the hospital:
- Developing the infrastructure facility so as to meet the growing demands of the out patients segment, as the hospital was designed to take care of the in patient.
- Establishing strategic alliances with some of the top profit making hospital.
- Giving better training and education to the staff so that they can be adequately utilized
- Offer better discounted bundle price/package to the patients so as to attract the insured patients as well. This will help increase the number of enrolments and increase the patient base.
- Increasing operational efficiency and reducing waiting time in the clinic.
- Reducing the dependency on funding and establish more ways to generate operational revenue
- Investing in technological advancements and providing high quality modern medical facilities to the patients
Directional strategies
The directional strategies are undertaken by the hospital to improve its position and enhance its reach and ability to serve maximum number of patients. Such strategies start with the defining of the hospital’s mission statement, vision, and goals. Healthcare centre is the leader to an evitable and just health care system through excellence, quality, compaction and trust. Some of the key value statements for the company are commitment to health and well being of those being served expectation, to achieve the highest level of excellence, understanding the vital importance of advocacy for those being served, imbibing creativity and innovation, recognizing the importance of working with the patients and the community and dedication towards providing high level education to health professionals.
Legislative-Political Changes
The Medicare program was established in 1965 to insure medical coverage for the aged and disabled. It then expanded to in compass other people entitle to social security or rail road retirement benefits and also people with end stage renal disease.
Another provision allowed non covered aged individuals to also benefit from the plan. There are 2 separate programs for Medicare i.e.
- Part-A :- Hospital insurance (free of charge)
- Part-B :- supplemental medical insurance (against monthly fee)
In 1997 Medicare as a whole covered 38 million people utilization of Part-A and B was 87% of enrolees. (DeButts, 1997). Title XIX of the social security act of 1965 gave rise to Medicaid as part of the federal state welfare structure to aid America’s poor population. It allowed federal funding for state run programs. In order to provide basic health service including hospitals in patients and out patients service laboratory and X-ray services and physician services.
Patient Flow System
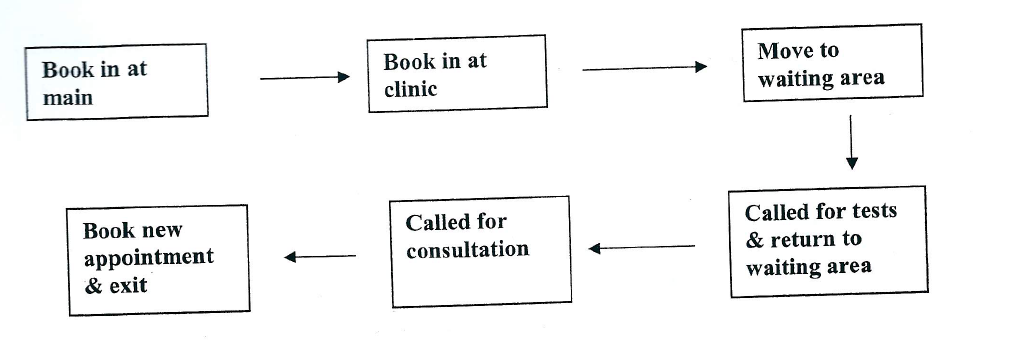
Employee Performance Gauge
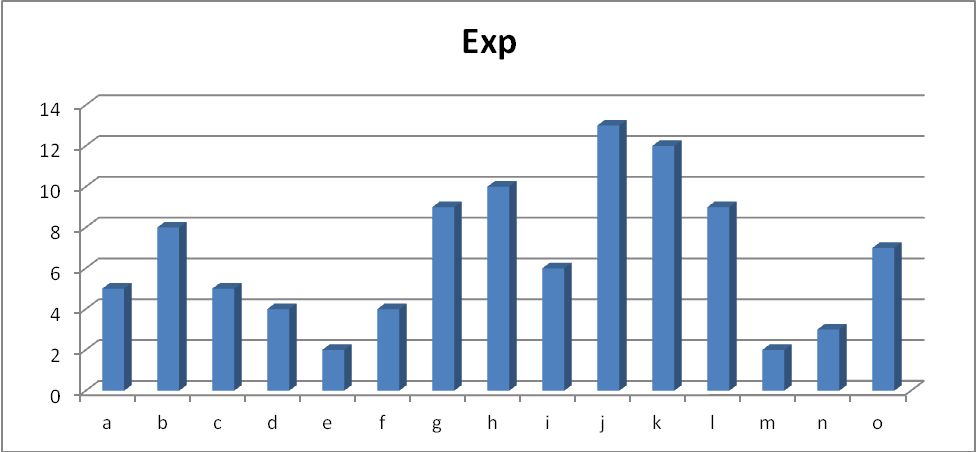
Experience of the employees is huge in the centre of the staff strength.
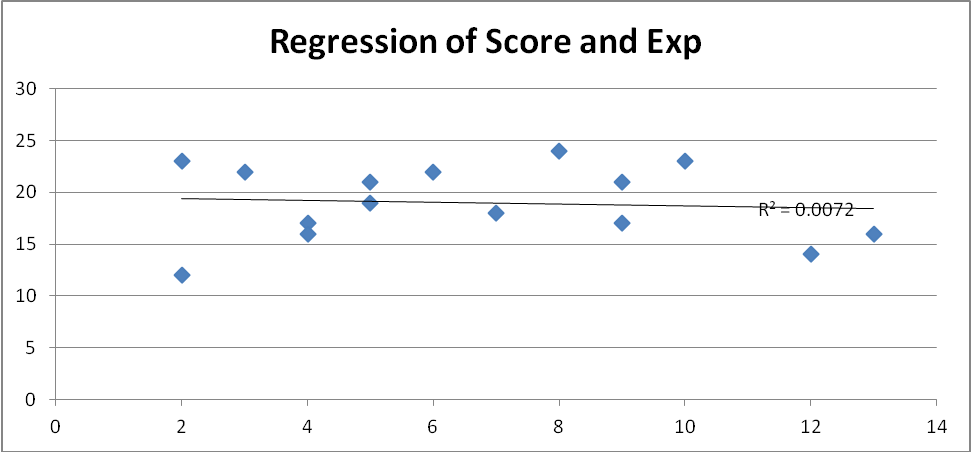
This is a regression test run on score in the test and the experience of the staff. This shows that there is no correlation in the same. Hence experience in the organization does not count towards the score in the test.
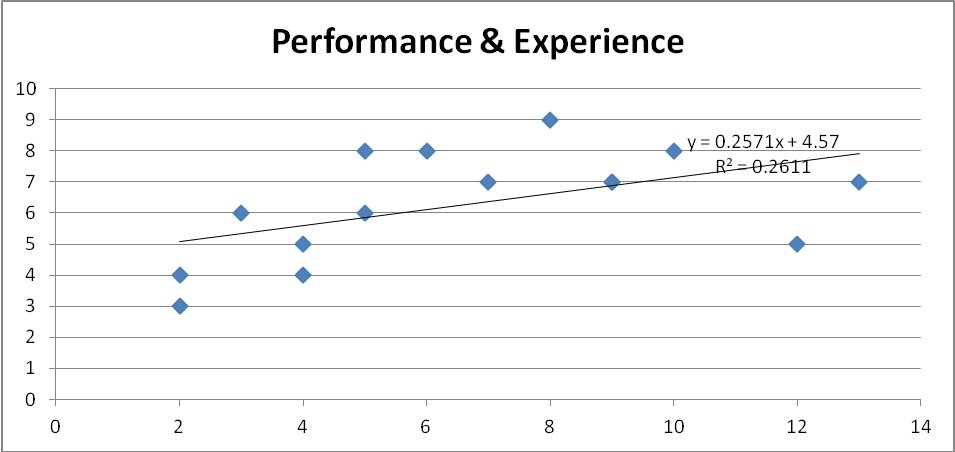
Further analysis suggests that there is a huge positive correlation between experience and performance at work. This can help us conclude that the questions in the survey are not good enough to gauge the performance of a work. Hence the methodology to measure employee effectiveness in that test is not appropriate.
Economic changes
Health care cost rose at twice the inflation rate from the mid 1980’s to mid 1990’s creating a 1 trillion dollars industry that accounted for 14% of the UK GDP. By the end of century the health care industry had grown to more than 1.5 trillion dollar or 18% of GDP. In 1995 nearly 3 quarters of English workers were insured by health maintenance organization, preferred provider organization and point of service plans up from only 27% in 1987(“The Economy in” n.d.).
Technological changes
In the 1990’s there was an increasing emphasis on outpatient care driven by the need to reduce cost and improve technology that would enable more types of care to be delivered on the outpatient basis.
The lack of capital resources with Rosemont to invest in technology enhancement, new medical renovation led to longer waiting time, patient frustration and declining enrolments. The shortage of examination rooms, clerks, nurses, and waiting room space further worsened the patients’ experience.
Sometimes the reason for this frustrated experience was the discourteous and uncompassionate behaviour of some people of the staff with the patients. There were some people in the staff who were very dedicated and loyal and compassionate but some were not interested in their jobs and used to perform below the expected levels and showed negative attitude to the patients. The administration made several attempts to improve the employee morale but it was of little use as there remained a core of negative people who demoralized other staff members and angered patients.
Competitive Changes
In order to provide good quality health care at affordable and fair prices to the poor and needy patients, the hospitals both Non Profit making and profit making should go in for a strong alliance and should complement each other’s competitive strengths and ensure to pass on the benefits of reduced cost, higher advanced technological developments, better quality health care to the indigent population. (DeButts, 2010)
Organizational Challenges
Establishment of cultural diversity in any organization itself is of great value and it has been observed that organizations that embrace such initiatives have been successful and growing. A diverse workforce enables company to offer solutions in a variety of ways ranging from service, sourcing and resource allocation. The diverse workforces bring with them talents and experiences in approaching solutions to problems and are adaptable to fluctuations in markets and customer demands. This diverse workforce also enables company to serve customers globally (Greenberg, 2004). The most important advantage of such workforce is the fact that such diverse workforce enables communication of varying viewpoints thereby providing larger pool of ideas and experiences (Goessl, 2008).
It’s an obvious and well known fact that when one aspect has benefits to offer and has support of a section of firm, it is bound to be opposed by some other section however small or large in nature on its belief that such an aspect or attempt will be not be in their benefit, which may or may not be true. Same applies when it comes to aspect of multi diversity in organizations.
The most common understood reason for this opposition to multi diversity practice is the fact that most of the people are comfortable with those counterparts who are like and behave like them and accepting diversity as a positive move is quite uncomfortable on their part (Jr., 1993). The other practical and important factor associated with this change is the fact that such change leads to development of encouragement of new approaches instead of old and troubling approaches.
Such a change gradual or sudden in nature for people accustomed to work in old ways become troubling and hence the resistance to change. Another critical problem with this approach is the fact that certain type or section of people might have prejudice against some section or group of people and to their discomfort that might find such a gradual change to be threatening due to one or many reasons. The reasons could range from simple disquieting acts or may be because they are of the feeling that at present whatever position they might be holding, they might find it extremely difficult to hold on to because of open competition for position instead of present positions of may be reservation systems for positions (Fernanadez, 1991).
We need to acknowledge the right words that R. Roosevelt Thomas Jr. said in his “Beyond Race and Gender” that in order to successfully implement a cultural diversity as a successful tool one has to look beyond the simple cultural diversity aspect to an outlook of active diversity management. He truly says that management of diversity is a managerial process which is comprehensive in nature in order to ensure that these changes act as a positive environment for all the employees experiencing it.
Diversity Challenges
Diversity management is also an inclusive process due to the fact that all employees belong to a particular cultural setup and it will include those who are among the traditionally strong cultural group in the old setup. The fact that needs to be appreciated is that diversity management is not just a job of us/them kind of management but instead it involves an approach of solution in which the solution being sought is resource management (Jorgensen, 1993). The approach undertaken should recognise, respect and preach the fact that other people’s standards and values associated with work are as valid as somebody from a completely opposite cultural set-up.
Hence management of cultural diversity id a prodigious task and it becomes more evident in areas where the cultural set-ups are more dominant. Because in such cases it has to be ensured that employees have o be made to believe and let go their old habits and ways and that too in positive way.
Internal Environment SWOT
Strengths:
- Pool of talented and compassionate staff members who choose to work at health systems and believed in its mission and enjoyed serving those in need.
- Turnover of the staff was pretty low
- Rosemont was considered one of the safety net providers across the US because of its mission to provide medical care to the poor.
Weakness:
- Declining revenue of the Hospital
- Majority of capital was funded and only 6% was operating revenue. With this low operating revenue, operations may become unsustainable in future
- Line of credit with bank was creating financial distress
- Hospital was not able to attract patients who are not insured
- Resources are not adequately utilized
- Inadequate infrastructure to take care of the growing demand in out-patients section.
Opportunities:
- Managed care was dominated form of insurance in US and enrolment was expected to increase
- Change in the US health care system. Managed care was altering how health care providers interacted with patients, funding for care was being restricted and many health care system were using non physician providers to cut cost. This threw plethora of opportunities in front of Rosemont
Threats:
- Vandalism and violence
- Stiff competition in the health care segment
- Technological advancements along with insufficient capital
- Inability to cope up with competition in the light of technological advancements which made diagnosis of multiple problems possible and insufficient capital
- Line of credit was missing, bankruptcy was nearing.
In a total compensation strategy compensation is based on different competitive levels of compensation. Performance based pay is a significant amount of pay for an executive officer. This policy helps in cutting down what is famously known as agency cost. This will insure that the executive officer works in the best interests of the shareholder, to whom he is an agent. This also ensures that salary costs are low in the case of a downturn. It helps in reduction of the cost without taking any drastic steps. It reduces retention risk and that too at a minimum cost to the shareholder and it also provides the management with a strong incentive to maximise shareholders’ value. The performance form of pay includes healthy bonuses, stock options and other incentive compensations. (Compensation Strategy, 2009)
Assessment of Role of Compensation in an organisation
Step 1
Competitive Dynamics
Tackling Competition is very important in any industry. It is the actual intellectual base of the company. Attrition rates are as high as 20% and poaching is always on mind of the competitors. HealthCare Centre has structured its pay strategy very competitively so that there can be minimum poaching possible from the organisation. (HealthCare Centre Compensation Plan, 2010)
Organization Culture/Values
HealthCare Centre has always been known for good team building. They have inculcated their values across the system and made sure that employees are happy so that they are encouraged to serve the customer in the best possible manner.
Social & Political Context
With geographically diversified base and employee strength ever increasing, it is now a whole circle that needs to be managed. Earlier, few selected employees and personnel used to be the key to the success of the organisation. In an environment where companies have global presence it is very important that social & political context of the residing country is adopted. HealthCare Centre has been known for keeping a very healthy look towards the social context of the country in which it is present.
Employee Needs
HealthCare Centre in its total compensation plan tried to make sure that all necessary needs of employees and their families are met with the compensation structure of the organisation.
Customization/Flexibility
HealthCare Centre has been flexible in its total compensation plan. It is upon the choice of employee to exercise the plan that deemed fit to him/her. They have also got customised travel holidays for employees residing in the United Kingdom.
Union Presence
There is no union present in HealthCare Centre.
Ethically human appraisal system can bring in bias from the leader of the team and hence it becomes very critical that it is very well designed. There is a well designed employee appraisal program which looks into the various aspects of appraisal of any employee. Employee’s engagement is another crucial factor. Employees should believe in work that they are doing and should always feel good about it. They should also understand the issues and problems confronting the company and work in harmony to overcome such obstacles.
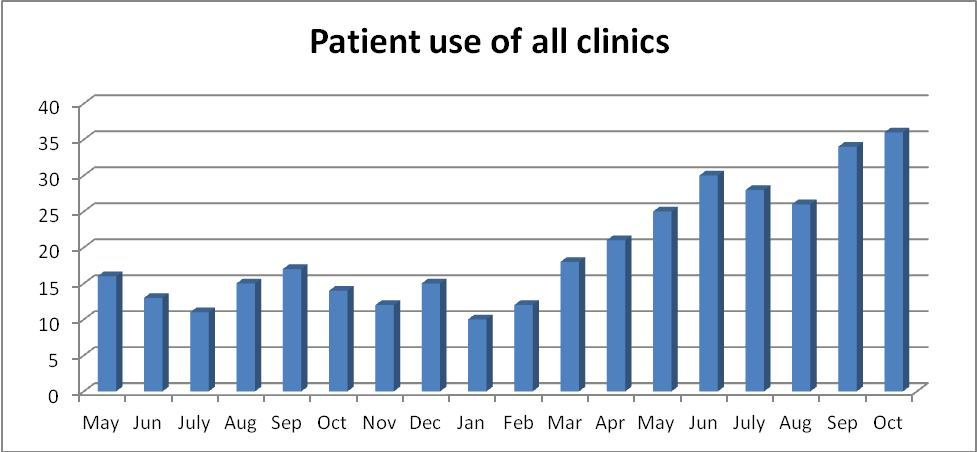
Capacity Expansion is required as the number of patients visiting out patient clinic is on a huge rise in the repeated months.
Personnel Management
‘Personnel management’ has developed into ‘human resource management’ over the years. This has happened because organisations are now not run by only the set of few people who calls all the decision. With geographical diversified base and employee strength ever increasing it is now a whole circle that needs to be managed. Earlier few selected employees and personnel used to be the key to the success of the organisation. With evolving times and unions of workforce becoming stronger it has evolved into Human Resource Management. Before developing a culture for an organization, it is very important to understand what culture actually means. Culture is all about dealing with your staff rather than your customers. This leaves a very positive note on the minds of the staff as they feel respected and being cared. Professional approaches to the non-performing side of the organisation were needed and clear accountability for all employees had to be established to ensure that all projects were properly staffed and completed on time and within budget.
An efficient leader is one who always has a fixed vision. He/she should be a good communicator so that he/she is able to express or communicate his/her views in the required manner. A good leader will always have a feeling of integrity towards the project undertaken. He/she should always be full of enthusiasm. His/her subordinates will take a lesson from his/her enthusiasm and will follow suit. This will help in timely completion of any particular project or task. An efficient leader should always have empathy towards his/her subordinates because there are other things besides work that people have to take care of. The leader should be able to understand their personal problems as well. He/she should be competent enough to handle any given task. Competency includes being well qualified and having complete knowledge pertaining to the task. He/she should be able to develop trust within his/her subordinates. The subordinates should feel that their leader is one of them. This way, the subordinates will be able to share their problems with the leader and as such, an emotional bond will be created. An efficient leader should have the skills to develop a team because without a proper team, no task can be completed successfully. The team will corroborate with each other to achieve the given task.
The success mantra for any successful leader is not to just have focus, clarity and good business plan but the ability to bring together a team of strongly motivated, determined and brave people is more important. Looking at these instances, it would be rather appropriate to classify his leadership style to be that of “bossing people around” which is a more abusive and unprofessional style of leadership. With the advent of changing technologies and growing competition, it has become imperative that employees should be motivated to learn new things and abandon old ideas. This can be done by a participative leader rather than an autocratic one. Though equally risky, this kind of authoritative attitude is required in a highly centralized and structured organization and during short decision making time.
Challenging cut throat competition, public relations & Human resource management (HRM) are becoming very critical for quick restaurant industry. In this context it becomes very critical to make sure that employees all over the world are happy. It becomes very important as we add on our base of our employees that we start following a standard procedure for recruitment and selection. Recruitment and selection will be happening all over the world as organisation is a MNC. The regions should be deciding when to recruit and where to recruit from. They are in best position to assess the capability of the work force in the region.
There are certain areas which have a great effect on a Community Pharmacy. Care should be taken while recruiting employees in a community pharmacy. The reason being the business is very delicate and full of responsibilities. A single negligence can cost someone’s life. So it is very important for the person to be well qualified and experienced. Since there is a dearth of well qualified and experienced people in the field of community pharmacy, the main problem is retaining the existing employees. Other pharmacies will keep trying to lure the employees by offering higher salaries. In retaining the employees, the management tactics and leadership qualities work wonders. The employees should be given frequent trainings so that they are familiar with the latest developments. The employees should be taught about the importance of time.
Expatriate Compensation Strategy
In an Expatriate compensation strategy compensation is based on different competitive levels of compensation. Performance based pay is a significant amount of pay for an executive officer. This policy helps in cutting down what is famously known as agency cost. This will insure that the executive officer works in the best interests of the shareholder, to whom he is an agent. This also ensures that salary costs are low in the case of a downturn. It helps in reduction of the cost without taking any drastic steps. It reduces retention risk and that too at minimum cost to the shareholder and it also provides management a strong incentive to maximise shareholders value. The performance form of pay includes healthy bonuses, stock options and other incentive compensations. (Compensation Strategy, 2009)
Business Strategy & Competitive Dynamics
Tackling Competition is very important in any industry like Information Technology where talent is the asset for the company. It is the actual intellectual base of the company. Attrition rates are as high as 30% and poaching is always on mind of the competitors.
At IBM there is enough encouragement to create big marketing strategies. The organisation is so huge that it implements strategy with a glocal (globally local) perspective. The organisation believes in globalisation and hence their marketing strategies are in sync with the thought process. The approach is truly professional and marketing methods are very well structured in sync with organisational goals. They consider HRM of utmost importance and their strategy is in line with organisational motive. Business culture of IBM is completely customer centric; hence their HR choices are very critical to organisational success. (IBM Expatriate Compensation Plan, 2009)
There is a well designed employee appraisal program which looks into the various aspects of appraisal of any employee. Employee’s engagement is another crucial factor. Employees should believe in work that they are doing and should always feel good about it. They should also understand the issues and problems confronting the company and work in harmony to overcome such obstacles.
Team Management Strategy
‘Personnel management’ has developed into ‘human resource management’ over the years. This has happened because organisations are now not run by only a set of few people who call all the decisions. With geographically diversified base and employee strength ever increasing it is now the complete circle that needs to be managed. Earlier, few selected employees and personnel used to be the key to the success of the organisation. With evolving times and unions of workforce becoming stronger it has evolved into Human Resource Management. Before developing a culture for an organization, it is very important to understand what culture actually means. Culture is all about dealing with your staffs rather than your customers. This leaves a very positive note on the minds of the staff as they feel respected and being cared. Professional approaches to the non-performing side of the organisation were needed and clear accountability for all employees had to be established to ensure that all projects were properly staffed and completed on time and within budget. (Human resource Management, 2007)
Training needed for Pharmacy Prescribing
In spite of the different models of prescribing prevalent in the UK and the wider international community, training programmers have always been compulsory for members of the varied healthcare professional before they are allowed to practice. At present, prescribing training is only available to qualified pharmacists with several years of professional practice experience although there have been calls for it to be included in the undergraduate training. “Although such course suggestions reflected pharmacists’ desire to improve their subsequent prescribing practice, diagnosis training may also be viewed as an important and distinguishing feature of IP…” (Cooper et al 2008). In accordance with the previous professional requirements, accreditation as a prescriber following successful completion of training has become the preserve of each profession’s regulatory body. In the case of pharmacy this was initially the Royal Pharmaceutical Society but from the year 2010 onwards it would be the General Pharmaceutical Council with the individual’s record being updated to include qualification as a non-medical prescriber. The professional record for the pharmacists includes the details such as the level of prescribing authority permitted, supplementary or independent pharmacist prescribing.
In the United Kingdom, national standards are followed while authorizing individual medical practitioners. On the contrary, in the United States of America, the various states have the authority to assess the competencies of individual medical practitioners and permit them to practice. Training for the pharmacists is multimodal and is being supervised by a higher education institution that provides face to face sessions and distance learning programme which is supplemented by part time practice, supervised by an independent prescriber. Both the higher education institution and supervised practice mode are very important as they allow the practitioner time to engage in clinical practice with the opportunity to apply the clinical knowledge from the distance learning course (Callum et al. 2010; Lloyd and Hughes 2007). A number of errors occur during prescription in medical practices mainly due to the increase in the frequency of prescription writing. The National Health Service records of 2000 show that during the year, $637 million worth of prescriptions were dispensed. The figure equals eighth part of the total National Health Service costs (The Audit Commission 2002). Even though the number of errors is increasing, prescription writing has become a neglected skill with little effort being dedicated for reducing the errors and improving patient outcomes. While a single action will not improve prescription writing, but a solution should be found to reduce patient’s harm and enhance confidence levels. Even though only a few researches have been done in the field of medical errors, several models have been suggested to explain the errors in the prescription writing. One model developed by Reason has gained some significance (Lloyd & Hughes 2007). The model mainly dealt with the risk factors causing prescription errors, from the perspective of individual, organization and external environment. In spite of the interest in studying prescribing errors, prescribing professions have faced significant challenges during prescribing. Studies show that there are certain deficiencies which happen during prescription practice in the doctors, nurses and pharmacists. There is shortage of committed professionals who could help students to gain invaluable skills in preventing this incidence of errors. Compounding this failure of prescribing is an over reliance on advice from pharmacists and nurses resulting in a high level of error. While in most cases the information provided is usually correct, this over reliance remains a major challenge (Callum, Carr, & Gray 2010). The new prescribing programmes have been incorporated to a great extent in training the fresh doctors as well as the practicing ones. It is mandatory for all the doctors to prove their competence before they get the practicing licence. As an important component of training, doctors are exposed to the important implications of inappropriate prescribing on the body’s functioning. The doctors should be able to interpret correctly the drug charts and prescribe accurate medicines and their doses (Barber et al. 2003). The use of modules relating to prescribing errors has been followed by pharmacists and nurses. While the doctors fail to correctly associate diagnosis with prescriptions, there has been much improvement in the recent past. In an effort to enhance the confidence in treatment, doctors are being encouraged to rely on the patient’s medical records when making prescribing decisions. Testing competency through this method has received widespread international support in the recent past.
With the introduction of new course guidelines (1980s), there has been reduction in much of the pharmacological education (Centre for the Advancement of Inter-professional Education 2000). Subsequently, with the adoption of intense practical lessons, the nurses were also required to prove their competence in a manner similar to that of the doctors. Following these changes, nurses have been given the right to prescribe a limited list of drugs under nurse formulary prescribing or extended formulary prescribing although this required qualification followed by examination. Some clinical nurse practitioners have become qualified to prescribe for patients suffering from hypertension and diabetes (Barber, Rawlins, & Frankin 2003). To ensure competence, the pharmacist have to be trained more than what is today. Previous studies have reported the importance of supplementary prescribing and support for reflective learning (Jones et al. 2007;Lloyd & Hughes 2007). But owing to the commitments towards work, the course duration is limited. The integration of the training of pharmacists with the other professions, such as nurses, undertaking non-medical prescribing in training programmes has generated debate. These multidisciplinary training programmes require an allowance to be made for the variation in training needs between the professions. Specifically, it is necessary for nurses to have an overall training and knowledge in pharmacology. This is in contrast to the pharmacists are mainly concerned with the relationship between the patient and the prescriber (George et al. 2006).
An emphasis on ensuring the detection of correct diagnosis in pharmacist training is crucial in prescription writing. In the hospital sector of pharmacy practice it has been estimated that 1.5% of prescriptions in general and medical wards have errors that are detected by the pharmacists (Dean et al. 2002). “Improving the resources available to the pharmacy department not only forms a core factor in the detection of errors but also would allow the pharmacy to increase assistance in correcting them” (Barber et al. 1997). Pharmacists are affected to a greater extent than the doctors or nurses due to lack of efficient and up to date information and knowledge. While concerted efforts are to improve the situation are being developed, pharmacists will continue to face barriers to practice especially in offering adherence support for patients (Cooper, Lymn, Anderson, Avery, Bissell, Guillaume, Hutchinson, Murphy, Ratcliffe, & Ward 2008d).
Multidisciplinary learning is a controversial subject that presents both benefits and problems to the health care professionals during training and subsequently in prescribing practice (Cooper, Lymn, Anderson, Avery, Bissell, Guillaume, Hutchinson, Murphy, Ratcliffe, & Ward 2008d). It is important that the inter-professional relationships accumulate the benefits which in turn result in a better understanding of the main professional ethics. This improves the communication with the patients and develops healthy relations (Elston 1996). Even though the reformation of the training system has been a topic of dispute, the stipulation of different skills in practice is not supported in actual practice. This has been demonstrated in the pharmacology trainings as well as the examinations of literacy. (Cooper et al. 2008b; Cooper et al. 2008c; Cooper, Lymn, Anderson, Avery, Bissell, Guillaume, Hutchinson, Murphy, Ratcliffe, & Ward 2008d).
“In addition, difficulties in compensating for the time spent gaining the necessary knowledge and experience prevent the incorporation into the undergraduate course” (Warchal S et al. 2006).
Implementation issues in Prescribing Practise
In spite of the introduction of supplementary prescribing earlier in the decade there was only a limited uptake of prescribing by pharmacists and nurses (Cooper, Anderson, Avery, Bissell, Guillaume, Hutchinson, James, Lymn, McIntosh, Murphy, Ratcliffe, Read, & Ward 2008c). At the most basic level this is represented by the inability of primary care clinical software systems to generate printed prescriptions for pharmacist prescribers. An inability to print prescriptions dramatically reduces the efficiency of pharmacist prescribing by enforcing handwritten copying of incorrectly computer generated prescriptions. This significantly increased the time required to issue prescriptions and due to the need to cross check prescriptions, there are unnecessary obstruction amidst efficient running of the prescribing clinic. Latest studies have revealed that there are barriers during implementation that pose complexities. These complexities have to be prevailed over while using information technology. This hints at multiple occurrences throughout the prescribing settings (Courtney et al. 2007; George et al. 2007; Weiss et al. 2006).
In pursuit of overcoming such problems, the care establishments and the principal care trusts have started promoting non-medical prescriptions in the principal care sector. At the same time as the non-medical prescriptions have become popular, the real practice has become restricted. This has happened due to the disparity of incentives being given to the principal medical care prescribers. In addition it was noticed that changes in medication, often suggested by pharmacists, did not lead to an increased role in prescribing but instead via patients’ medical records. While nurses and pharmacists have made some progress in getting into actual prescribing practice more effort is required if the dominance of medical profession is to be challenged (Cooper, Lymn, Anderson, Avery, Bissell, Guillaume, Hutchinson, Murphy, Ratcliffe, & Ward 2008e). In view of the above a review of the implementation of pharmacist supplementary prescribing for hypertensive patients in the community found that the inaccessibility of patients’ records, inadequate funding and poor relationships among the medical and pharmacy professionals were the main problems preventing more widespread application (Weiss, Sutton, & Adams 2006). The distortion of relationships between the prescribing pharmacists and their patients whose common view of pharmacists as shopkeepers rather than healthcare professionals further handicaps the implementation of pharmacist prescribing in the community sector (Hughes and McCann 2003). The perpetuation of such barriers and the now largely inappropriate perception of pharmacists are regrettable when there are clear advantages, opportunities and benefits for both the patients and the prescribing pharmacists (Cooper, Lymn, Anderson, Avery, Bissell, Guillaume, Hutchinson, Murphy, Ratcliffe, & Ward 2008e). A greater involvement by pharmacists would have a significant effect in the promoting and overall success of the supplementary prescribing initiative (Cooper, Lymn, Anderson, Avery, Bissell, Guillaume, Hutchinson, Murphy, Ratcliffe, & Ward 2008e).
There are concerns that situational violations of the clinical management plan requirements could impact directly on the overall safety of the supplementary prescribing process. It has been said that the clinical management plan represents a necessary level of reassurance of safe practice while providing guidance for the pharmacist and nurse prescribers (Cooper, Lymn, Anderson, Avery, Bissell, Guillaume, Hutchinson, Murphy, Ratcliffe, & Ward 2008e).
Ineffective planning on the behalf of healthcare authorities restricting or delaying access to prescribing training has resulted in barriers to the overall development of non-medical prescribers careers particularly in the nursing profession. “Overcoming these barriers while emphasising interaction with the medical profession during supplementary prescribing provided much needed confidence for nurses particularly when dealing with complex problems” (Courtenay, Carey, & Burke 2007).
Patients have accepted the role played by nurse prescribers in the primary care sector, particularly in the area of managing the treatment of patients with hypertension. It is essential that the support and appreciation of patients is achieved in the implementation of non-medical prescribing practice within both primary and secondary care sectors (Cooper, Lymn, Anderson, Avery, Bissell, Guillaume, Hutchinson, Murphy, Ratcliffe, & Ward 2008e). Independent prescribing is still viewed by many patients as being the preserve of the medical profession and this leads to a cautious approach to the introduction of changes to complex medication packages by other professionals. Generally, patients appreciate the pharmacist involvement in a prescribing role showing a positive attitude especially after experiencing treatment by them. While the majority of the public would still prefer visiting a medical practitioner for treatment, the contribution of pharmacist prescribers is generally supported with a willingness to recommend the service to friends (Stewart et al. 2008).
Key Targets – Hypertension Surgeries
During 2008 there were one thousand one hundred and forty seven appointment slots scheduled although only nine hundred and sixty nine were available for hypertension patient consultations. The difference in the figures represents the scheduled sessions allocated for routine administration; catch up time and to allow for prescriber breaks during the session. Over the year there were one hundred and eighty seven appointments that were still available to be booked at the scheduled time representing approximately nineteen percent of the total appointments. Of the unfilled appointments, one hundred and seven, or eleven percent of the total appointments, were due to cancellations. With the age of the patients being consulted there was an enhanced risk of cancellation. Cancellations could be due to various causes such as, adverse weather conditions or the need to attend hospital appointments hence the high number of cancelled appointments. Four percent of the total numbers of appointments were missed by the patients, classified as did not attend on the clinical system, which in view of the age distribution of the patients is not unsurprising as forgetfulness increases with age (Hanninen and Soininen 1997). Ten percent (or seventy three in number) patients arrived after the scheduled start of the appointment time and the average patient waiting time over the year was nine minutes after the scheduled start time. Forty six percent of appointments were started on time or within five minutes of the scheduled start time and forty three percent of appointments ended within the allocated appointment time. While the large majority of the patients seen in the pharmacist hypertension clinic were registered by the National Health Service with the medical centre two were temporary residents. These temporary residents required the urgent supply or a prescription to allow them to continue treatment prescribed elsewhere but left at home when coming to visit Highcliffe on holiday.
All the patients seen were over the age of sixteen years with seventy nine, ten percent, being aged seventeen to sixty four years and the balancing ninety percent being sixty five years or older. Of the patients referred to the pharmacist hypertension clinic twenty six percent did not need to be seen more than once, indicating that their blood pressure targets had been achieved when seen. This high proportion could be due to patients being more at ease when their blood pressure was recorded in the pharmacist clinic or having increased adherence with previously prescribed antihypertensive medication. The majority had been referred as the result of a raised blood pressure reading taken a few days previously by the medical centre health care assistants.
Approximately forty two percent of patients were seen twice indicating that prescribing changes quickly achieved target blood pressure levels for these patients or that they were previously not regularly taking their antihypertensive medication. Failure to adhere to an agreed treatment plan is common among older patients suffering from asymptomatic conditions like hypertension (Hyre et al. 2007). It is standard practice to review the effect of prescribing changes one month after the introduction of a new medication or dose change in an existing medication. However, in cases of severe hypertension review at a shorter interval is necessary and these would normally be treated with a supporting general practitioner.
Sixteen percent of patients were seen three times, a further six percent required four appointments, and seven percent needed to be seen five times. The remaining three percent of patients required either six or seven appointments during the year. The high number of appointments for these last two groups of patients being due in part to a six monthly repeat review of blood pressure or a need to change medication for patients who report adverse reactions to prescribed treatment.
The age distribution of hypertension patients for which new medication was prescribed by the pharmacist approximately reflected the age profile of hypertension patients at the Medical Centre. Ten new prescriptions were issued to patient in their fifties, twenty three in the sixties, sixty five in the seventies, sixty four in the eighties and six to those in their nineties. Fig 1 shows a graphical comparison of patient age for prescriptions issued and ages of patients on the hypertension register.
Inappropriate prescribing
It is very important for the medical practitioner to carefully diagnose the disease and prescribe appropriate medicines. Such attentiveness, timely diagnosis and treatment can help in avoiding deaths due to diseases that can be prevented. It is a fact that monitoring the administration of medication and its effect for quality control purposes is much more difficult, and indeed rarely attempted, in the community environment with ambulatory patients when compared to inpatient drug therapy. It is clear that inappropriate prescribing does contribute to the increasing levels of adverse drug reactions seen. Assessment of case studies has revealed that wrong prescription of medicines has been a risk especially to the health of the aged when it could have been avoided (Herbert, Wright, Maclure, Wakefield, Dormuth, Brett-Maclean, Legare, & Premi 2004). Lack of follow-up in cases of hypertension were identified whether due to failure of process or negligence which when considered with the known increased risk of stroke and myocardial infarction associated with hypertension should have been avoided. Patients are hampered due to vast numbers of errors in prescribing. Two main areas which cause the researchers particular concern are the use over addictive drugs rather than safer alternatives and the continued use of ineffective drugs which resulted from the effects of several of the decision influencing factors (Soumerai et al. 1989). Data from clinical trials is being used as benchmark during medical practice. But unfortunately, like the Chinese whisper, the information travelling from the clinical research to the actual practice is thinned or in other words, does not have the accuracy. Prescription patterns in hypertensive patients when examined were found to show a failure to widely integrate the beneficial findings from clinical trials (Stafford et al. 2006). In recent studies on antihypertensive medication it has been noted that the appropriate combination of a variety of effective treatments, despite being at minimal doses, can achieve control of blood pressure with a decreased incidence of adverse effects (Kotchen 2006). This advantage from the combination of an effective treatments at low doses was also supported by findings of a study conducted during the period of 1999 to 2002 which demonstrated an increasing use of multiple antihypertensive drugs and a sharp reduction in the reliance on mono-therapy (Gu et al. 2006).
Key Observations noted during the Case
It is an unfortunate feature of the introduction of non-medical prescribing that it has increased inter-professional rivalry between the medical, nursing and pharmacy professions. Upgrading of the non-medical prescriber training to a multidisciplinary format in response to the differing needs of each healthcare profession has resulted in a better understanding of non-medical prescribing. In recent years the increased application of evidence from clinical trials has become a common phenomenon in prescribing practice and this promotes improved patient health through reduced morbidity and mortality.
The implementation barriers experienced by non-medical prescribers starting supplementary prescribing practice persist hindering the nurses and more significantly the pharmacists in participating in their prescribing role. Despite this enough experience has been gained to show that wide support and appreciation by patients treated by pharmacist prescribers has bolstered the confidence of these pioneering pharmacists. The attitude of patients towards pharmacist prescribing is affected by the persisting view of community pharmacists as primary businessmen and this is believed by some to influence their prescribing practice.
Key Observations – “Condition prescribing on a Long Term Basis”
Different medical practitioners have different way of taking care of their patients who suffer from a variety of ailments. Normally, the kind of plan to be followed during the course of treatment of a patient depends on certain factors like the kind of disease, the financial aspects of the patient, and the medical system of that particular country or state, etc. There are certain chronic diseases like Diabetes in which the patient is supposed to follow a predetermined plan. Such plans may be supervised by the prescribing pharmacist or a nurse along with a prescribing doctor. It has been a matter of grave concern while applying the predetermined plans in instances where the patient suffers from hypertension. The efficiency of a predetermined health plan has been argued due to the fact that such a plan is supposed to be helpful in successfully curing or controlling the ailment (Berlowitz et al. 2003). The arguments have resulted in doing a relative study in order to judge the various health care plans available. The motive of the study is to evaluate the results of such plans in 100 patients of hypertension. These patients have been divided in three groups. The first group shall be observed by a non-prescribing nurse under supervision of a prescribing doctor who will not be in the patient’s direct touch. The second group shall be observed by a healthcare assistant who is not as qualified as the nurse and will be under the supervision of a prescribing doctor. The third group shall be observed by a self-determining prescribing pharmacist.
Close to one in “every five Americans suffer from high blood pressure, making it the country’s most prevalent medical condition” and it is expected that this situation will be closely followed by the population of Western Europe (Berlowitz, Ash, Hickey, Glickman, Friedman, & Kader 2003). Traditionally it has been believed that one half of individuals with the condition are not aware that they have it, half the patients identified are not treated and half of these do not have controlled blood pressure (Cranney et al. 1998). According to reports of the WHO, hypertension is third most observed reason for human deaths in the world. If hypertension is not treated timely, it may result in heart diseases such as heart stroke and coronary heart disease (Duggan et al. 1997).
Such diseases are supposed to be silent killers because there are no symptoms and the problem surfaces only after the damage of that particular organ has started. It is heartening to know that there are millions of people who suffer from undiagnosed hypertension and among those, in whom hypertension has been detected, 42% are supposed to be getting wrong treatment (Twinn et al. 2010). The treatment for patients of hypertension is aimed at lowering their blood pressure so that the threat of a heart attack is minimised or averted. “To manage this condition, modification of a patient’s way of life is usually regarded as the primary treatment method for blood pressure at a high normal level” (Schroeder et al. 2000).
In case the suggested change in lifestyle is unable to lower the blood pressure, appropriate medicines are prescribed. Usually, such prescriptions are made for patients suffering from extra ordinary high blood pressure and other diseases such as diabetes and heart ailments.
A health plan should actually be designed in such a manner that the patient is able to accomplish a suggested Body Mass Index (19 to 25) and become capable of walking briskly for at least thirty minutes on a daily basis (Robinson 2000).
However, if the patient has other conditions they should consult their doctor on the type and level of exercise that should be attempted. Hypertensive patients should be advised to eat a diet that contains fresh fruits and vegetables; it is now thought that to include at least five portions of these on a daily basis is ideal. Reduce fat intake by replacing full fat dairy products with their, low fat dairy equivalents and generally reduce the fat content and especially saturated fat in the diet (Menard and Chatellier 1995). The plan should restrict the patient from consuming canned food and alcohol and from smoking. The patient should use the drugs (without fail) prescribed by the doctor.
A crucial part of patient management and thus the health care model used should ensure that the patient is provided with effective antihypertensive drugs “that will lower the blood pressure and prevent complications that are linked to hypertension” (Loveman et al. 2003). A reduce in the blood pressure will enable the patient to live a happy and enjoyable life. Some patients might find the hypertensive drugs to be expensive. As such, it should be the duty of the doctor or the pharmacist to find out an economical alternative or substitute (Duggan, Ford, & Eccles 1977). The prescribing doctors or the prescribing pharmacist are very crucial to any health plan because they are the ones who deal with the patient and they only know the exact condition and level of the patient’s hypertension. They are the ones who suggest a particular health plan for the patient. The plan should be such as to improve the patient’s life’s quality. In addition to the doctor or the pharmacist, there are other people who have important roles to play in successful completion of a health plan. They have to maintain a fruitful relationship between the patient and the various options available for a successful treatment. There may be patients suffering from hypertension who may be unaware of the “clinical resources that are available to ensure the successful implementation of treatment strategies” (Laurant et al. 2004). It has been suggested by various researchers that more medical professionals should get themselves engaged in the supervision of hypertensive patients. According to them, the professionals engaged in the treatment of hypertensive patients should work as a team and corroborate towards the successful treatment (Fahey & Lancaster 1995). By doing so, all the works can be done without fail such as if a pharmacist doesn’t know what to prescribe in a dietary plan he/she can refer to a dietician for appropriate prescription. Dietary plan forms a major part of the health plan in case of a patient with hypertension. It has been observed that by following a proper dietary plan, patients with hypertension have been able to attain the required Body Mass Index by curtailing the ingestion of salts (Horrocks et al. 2002).
As such, a new management system in treating patients with hypertension has been evolved wherein the roles of different health care professionals have been enlisted. “However, there is not much data to indicate that indeed a one dimension approach compromises the quality of service” (Anon 2010). Also, “Available data only points towards the effects associated with failures of the different treatment regimens. For example, it is generally accepted that the major obstacle to achieve improvement in cardiovascular disease morbidity and mortality is the failure in complying with the therapeutic dietary changes”. (Cranney, Barton, & Walley 1998).
Apparently, the health provider needs to be analysed properly. Such instances where the health provider is not in direct touch with the patient have been disapproved of. When a doctor relies on the information and feedback about the patient from an assistant who is not well qualified, there ought to be a bad effect on the treatment being provided. According to a study carried out in Hong Kong and aimed at analysing the results of different health care plans meant for hypertensive patients, it is the nurse who contributes the greatest towards the care of the patient (Twinn, Lee, Lam, Thompson, Cheng, & Goggins 2010). The patients observed under this plan showed a swift decrease in BMI in one year. Owing to the enormous experience of the nurses, the APN plan was observed to be offering improved services. “The findings also pointed towards deterioration in quality of services from the traditional model of care”. (Fahey & Lancaster 1995). “In previous related researches patient perceptions are seen to be influenced by factors that determine their perceived need for service, specifically their perceived health need at the moment of consultation” (Cranney, Barton, & Walley 1998). It is understood that patients wish to talk to their doctor about the prescriptions but when the plan involves a doctor who doesn’t have to be in direct contact with the patients, the patients get annoyed or even disheartened and as a result give pessimistic feedback for that particular plan. “In another study it was revealed that the general management of hypertensive patients had improved considerably due to involvement of different health care professionals”. (Duggan, Ford, & Eccles 1997). The study aimed at determining the blood sugar levels of two third patients who were 65 years of age and more. These patients were treated for their increased blood sugar levels. But not all of them had increased levels of blood sugar. The results of the study demonstrated marvellous improvement as compared to the data from earlier studies. The results of the study pointed towards a substantial disparity between “practices in numbers of older hypertensive patients who were treated and had their hypertension controlled” (Loveman, Royle, & Waugh 2003). “An unpopular finding was also registered in a certain study, in which the doctors’ negative attitude was found to be a major factor that may contribute to suboptimal management of older patients” (Fahey & Lancaster 1995).
A survey conducted on the general medical practitioners showed that there are various factors responsible for a doctor’s unwillingness to provide optimum treatment to patients with hypertension and as a result increase their afflictions. The specific factors identified include the “fear of adverse effects and lack of appreciation of both risks of untreated mild hypertension in this age group and appreciable life expectancy of people aged 60 years and above” (Fahey & Lancaster 1995).
Observations – Prescriptions issued in Pharmacist-led Hypertension Clinic
During 2008 the pharmacist wrote one hundred and ninety three prescriptions all of which were entered into the Medical Centre clinical system as repeat items with six repeats for one month’s medication being prescribed. The pharmacist therefore authorised one thousand one hundred and fifty eight prescriptions although some of these were changed at subsequent follow-up appointments. The majority of new antihypertensive treatments prescribed, one hundred and twenty three prescription items, were still being issued to patients when reviewed in December 2009. These continuing repeat issues currently represent over two thousand two hundred prescription items. Twenty one prescribed items were subject to dose increases and six to reduced doses when reviewed in December 2009. Six antihypertensive items prescribed were switched from one angiotensin converting enzyme inhibitor drug to another due to a prescribing policy change.
Seventeen items were discontinued by December 2009 due to side effects, intolerance or allergy. Five items were discontinued as no longer required and a further six discontinued without a recorded reason.
One patient refused to take antihypertensive medication and was responsible for the discontinuation of a further seven antihypertensive items prescribed in the clinic. Two patients treated in the clinic were lost to follow-up, one moved away and the other died in hospital with the cause of death recorded as pneumonia. The following two graphical representations show the fate of items initiated in the pharmacist led clinic (Fig. 3) and the reasons for discontinuation of prescription items which were stopped by December 2009 (Fig. 4).
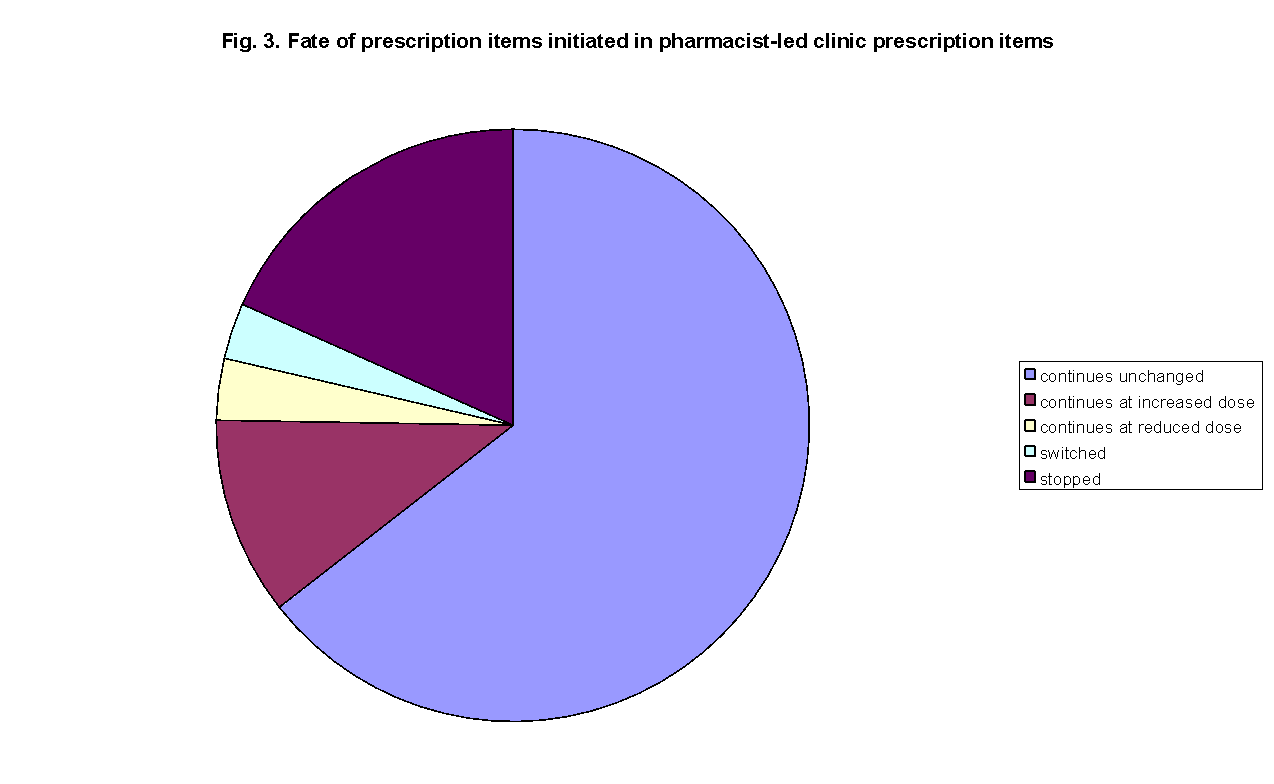
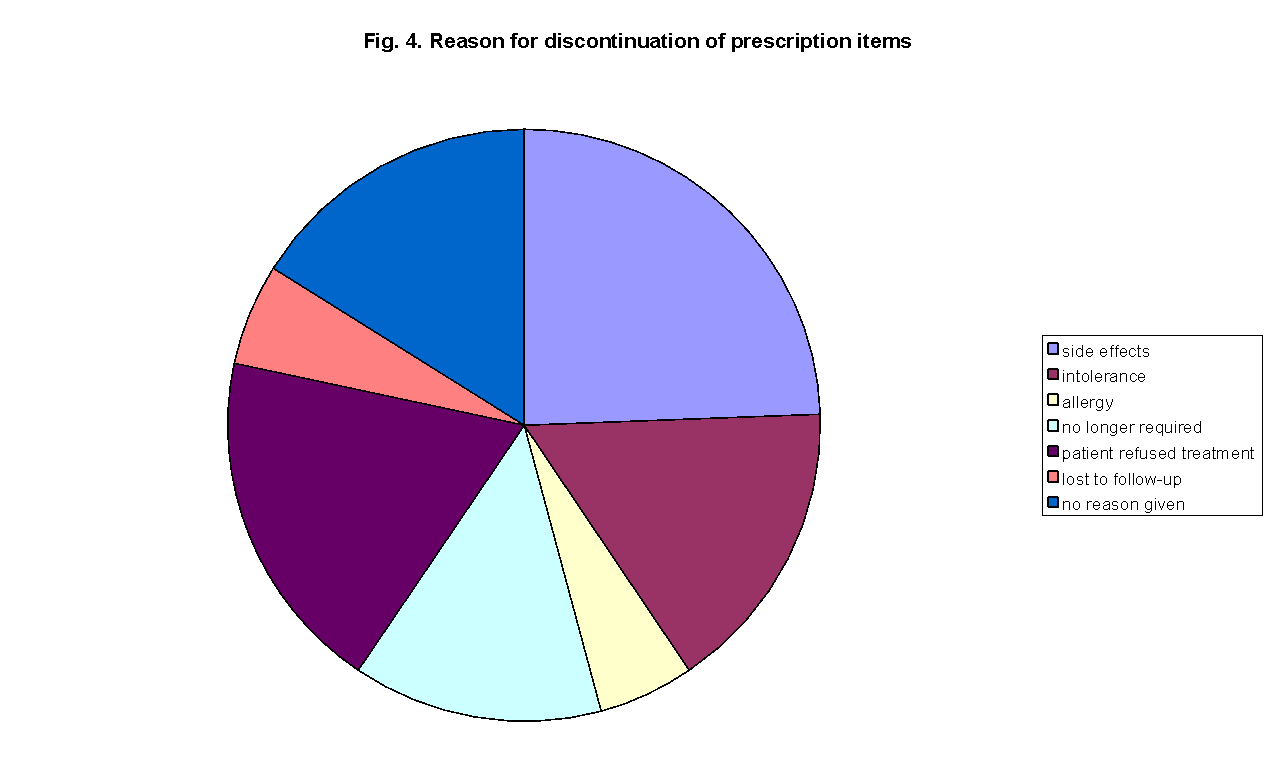
Anti-hypertension prescriptions issued by pharmacist prescriber
“The need for physicians to remain up-to-date with regard to improvements in drug treatment, procedures, and diagnostics is of great importance” (Siegel et al 2003). The most frequently prescribed group of anti-hypertensive agents were those acting on the angiotensin-renin system. This group consists of the angiotensin converting enzyme inhibitors and the angiotensin receptor blocking drugs. Calcium channel blocking medicines were prescribed with similar frequency to thiazide diuretic drugs with use of beta-blocking medication being much less common. The relative frequency of prescribing each of the major antihypertensive medication groups is represented in Figure 5.
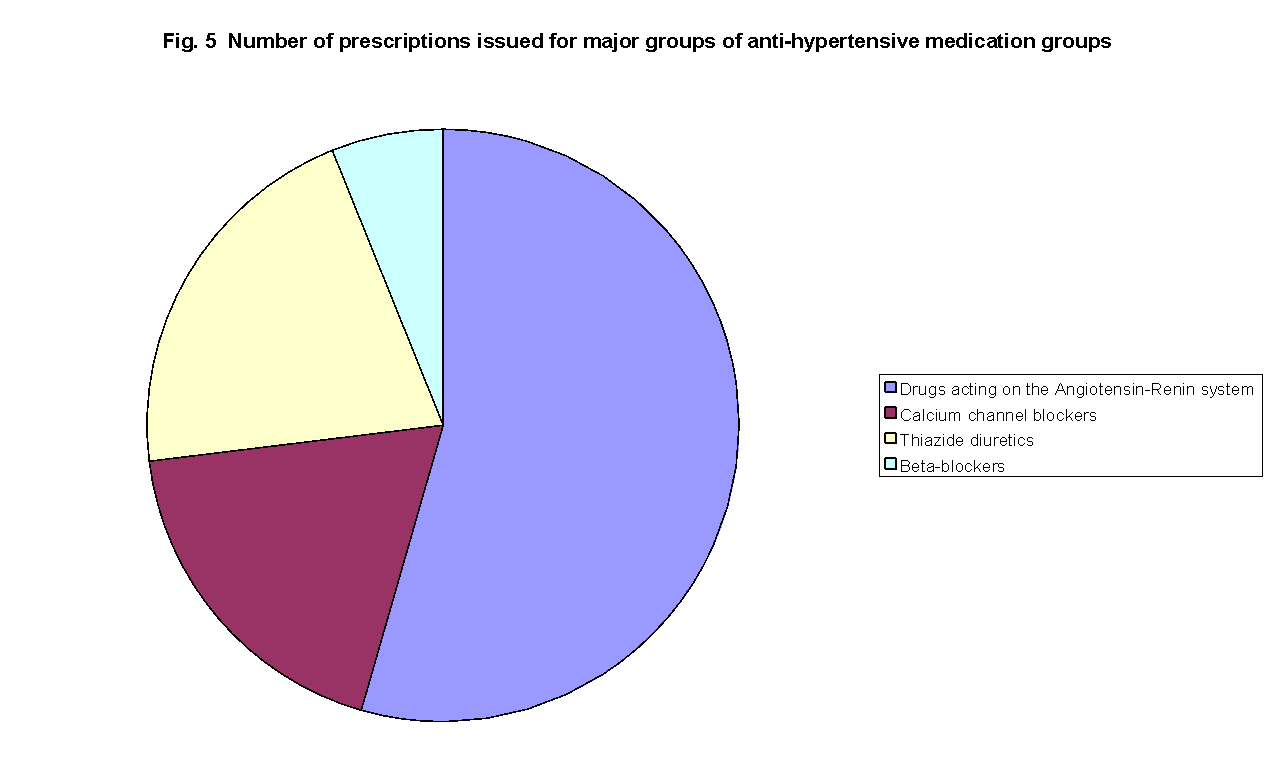
It can be seen that the majority of prescriptions were issued for drugs acting on the Angiotensin-Renin system and this may have several explanations. Due to the age of the patients being treated in the pharmacist-led clinic many patients had some degree of chronic kidney disease as revealed by renal function blood tests. The current guidance for the control of blood pressure in patients suffering chronic kidney disease encourages the use of drugs acting on the angiotensin-renin system (National Collaborating Centre for Chronic Conditions 2008). There is a link between type 2 diabetes mellitus and kidney damage and as a result of an apparent protective effect against future kidney damage the drugs are routinely used to protect patients with diabetes (HOT Study Group 1998). These patients are at a higher risk than average of cardiovascular disease and a study investigating the benefit of using a rennin-angiotensin system drug, ramipril, in a group of 9297 patients found a reduction in cardiovascular death of twenty six percent (Yusuf et al. 2003).
These drugs are available in a range of doses and it has been common practice in the pharmacist-led clinic to start patients on the lowest dose and increase dose as necessary to achieve control of the patient’s blood pressure, the start low, go slow approach to medication changes in elderly patients (Sherman 2009). This start low, go slow approach and the range of doses available in these drugs partially explain the apparent bias towards prescribing them. The use of these drugs has been increased with practical experience of the low incidence of serious side-effects when prescribing them. The most common adverse effect has been the angiotensin converting enzyme inhibitor cough which is thought to affect between ten and twenty percent of patients. This adverse effect is rarely experienced by patients taking the newer angiotensin receptor blocking drugs. However, the clinical trial evidence supporting the use of angiotensin-renin system drugs is largely based on the angiotensin converting enzyme drugs and therefore it is standard practice to prescribe these in preference to angiotensin receptor blockers.
Drugs Blocking Calcium Channel
This was the second most frequently prescribed group of drugs in the pharmacist-led hypertension clinic. There are two major groups of calcium channel blockers, the dihydropyridines which are usually used to treat hypertension and the non-dihydropyridines which are most commonly prescribed to patients with a history of angina or heart attack. Dihydropyridines reduce blood pressure by dilating blood vessels and therefore reducing resistance to blood flow through the peripheral vascular system. In contrast the non-dihydropyridines act mainly through reducing the heart rate and reducing the degree of heart contraction. The purpose of both of these actions is to reduce cardiac output and this, therefore, reduces blood pressure. Studies into the use of Calcium channel blockers have shown that they are particularly effective in treating isolated systolic hypertension, that is when the systolic blood pressure is raised but the diastolic pressure is normal (Staessen et al. 1997). Isolated systolic hypertension is a common feature in elderly hypertension patients as the often age related increase in arterial stiffness has a greater effect on systolic blood pressure than diastolic.
In the pharmacist-led clinic no patients were started on non-dihydropyridines by the pharmacist although for one patient already taking one of the drugs the dose of one of these drugs was increased. In contrast to the rennin-angiotensin system drugs, calcium channel drugs have been found to cause more adverse effects in patients. Ankle swelling, flushing and postural hypotension (low blood pressure that is related to posture) had been the most commonly reported adverse effects. It was the experience of the pharmacist prescriber in discussing treatment options with patients that the potential side-effects of calcium channel blockers were considered less acceptable than those for renin-angiotensin system or diuretic drugs. This reluctance to risk ankle swelling or flushing was largely responsible for the fact that calcium channel blocking medication was started so much less frequently than renin-angiotensin system drugs.
Thiazide diuretic drugs
Thiazide diuretic drugs were the third most commonly prescribed anti-hypertensive drugs used in the pharmacist-led hypertension clinic. These diuretic drugs have been used to treat hypertension for many years having been introduced in the 1950s. At first it was common to prescribe two strengths of thiazide diuretics for hypertension but experience has shown that doubling the dose increased adverse effects more than anti-hypertensive effect. The Medical Centre formulary has as the first choice thiazide diuretic Bendroflumethiazide and the dose of 2.5 mg each morning is the only dose prescribed in the pharmacist clinic.
The use of thiazide diuretics is considered to be the first choice for patients over the age of 50 with uncomplicated hypertension; a recommendation supported by one of the largest clinical trials of hypertension treatment ever conducted (The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group 2002). The main reason for the relative numbers for new prescriptions issued in the clinic for thiazide diuretics is that most patients were already under treatment for hypertension with a diuretic. A secondary reason for the lower number of diuretic items prescribed is that only one strength of diuretic medication was prescribed in contrast to other anti-hypertensive medications which all have several different strengths in regular use.
Beta-Blocking drugs
The prescribing of beta-blocking drugs has been a minor feature in the pharmacist-led clinic. This is due to a change in emphasis from the third version of the British Hypertension Society guidelines and the more recent fourth guidelines. Under the new guidelines beta-blockers are not recommended as first choice medication for simple hypertension although they remain an appropriate treatment for patients with a history of angina or heart attack.
Most of the prescriptions for beta-blockers initiated in the clinic were for reduced doses during managed change from beta-blockers to alternative treatments. A significant influence on these switches from beta-blockers to other types of anti-hypertensive treatment have been in response to newspaper reports of long term risks associated with beta-blockers (Laurance 2008).
Observations – Outcomes of prescribing by pharmacist independent prescriber
Following the initiation of a new anti-hypertensive medication prescription by the pharmacist prescriber one hundred and eleven patients achieved their target blood pressure levels when it was taken at a follow-up appointment. There were forty nine patients who did not achieve control of their blood pressure by the time of their next blood pressure clinic consultation. The majority of these patients whose blood pressure remained above target were given further prescriptions at their follow-up consultation either for increased doses of current medication or for additional medication. After dose increases or the use of alternative treatments twenty eight of these patients did achieve blood pressure targets. Of the remaining twenty one patients, five were recorded as being on the maximum tolerated dose of antihypertensive therapy after all the possible treatments had been either trialled or discussed and declined by these patients. One of the hypertension clinics’ most frequently seen patients eventually admitted to being unwilling to take anti-hypertensive medication. He was therefore recorded as refusing treatment and offered an appointment to discuss future treatment of his hypertension whenever he felt ready. A further three patients were referred to the general practitioners at the Medical Centre for treatment. Two of these referred patients had developed heart failure requiring treatment with medication outside the clinical management plan that had originally been agreed with Dr. Collins. The third patient’s blood pressure could not be controlled with the range of medication that had been agreed as appropriate for use in the hypertension clinic. As the pharmacist felt that he did not have sufficient experience in prescribing alpha-blocking medication or centrally acting antihypertensive, this patient was also referred to a doctor for further medication. There were twelve patients whose blood pressure were still uncontrolled at the end of 2008 and required further treatment in the clinic during 2009. The majority of these patients achieved target blood pressure levels during 2009. The outcomes of treatment of patients seen in the pharmacist-led hypertension clinic are graphically represented in Fig. 6.
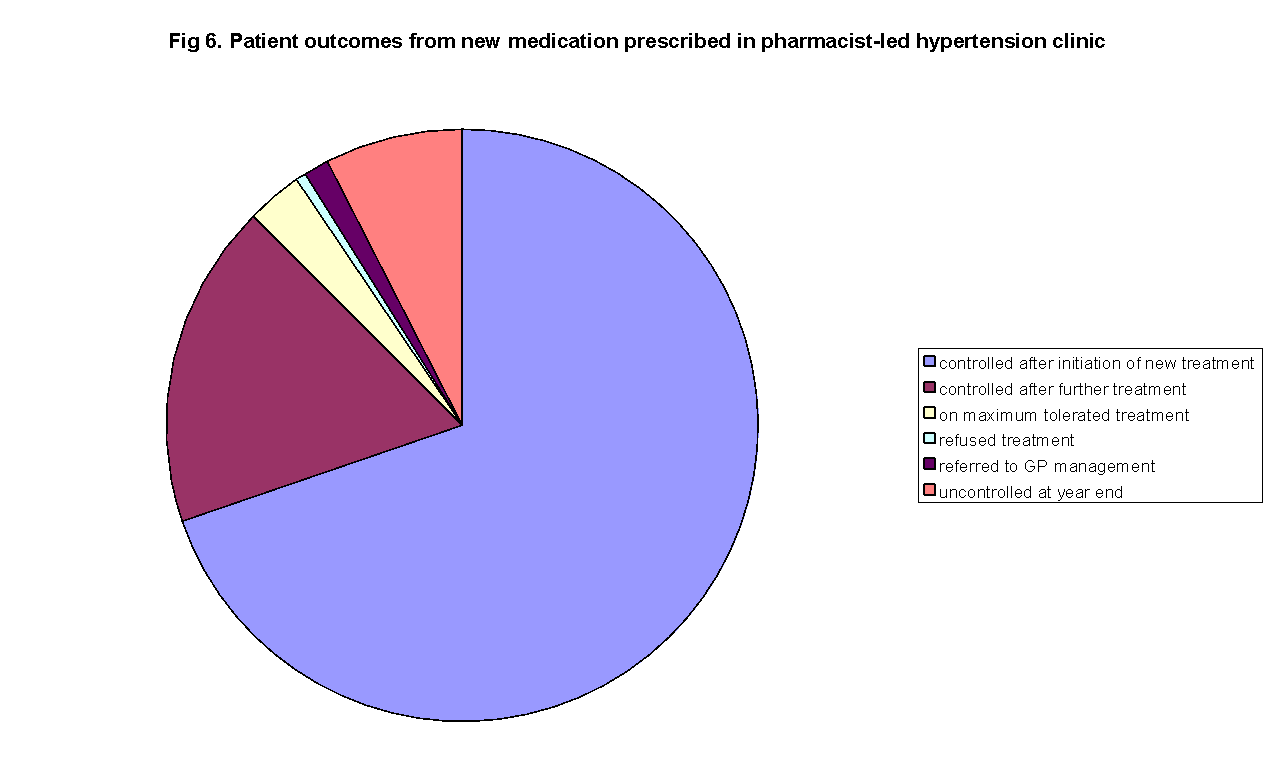
The overall performance of the pharmacist-led hypertension clinic can be seen in Fig 7 which shows the proportion of patients whose blood pressure was within the target levels when seen in the clinic. This graph includes those patients who were found to have blood pressures at target levels when first seen by the pharmacist prescriber and those whose pressures returned to target levels without any increase in treatment. It can be seen that ninety four percent of the patients seen in the clinic achieved target level with the remaining being referred to the Medical Centre doctors for further treatment or excluded from blood pressure targets.
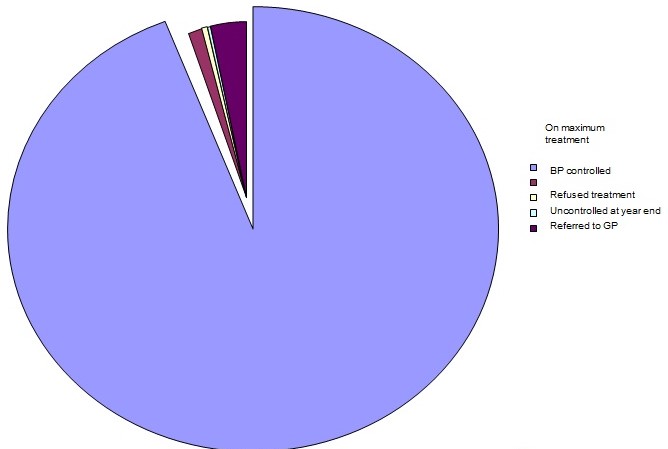
It can be seen from Fig. 6 and Fig. 7 that the patients seen in the hypertension clinic had through rechecking of their blood pressure, healthy lifestyle advice or changes to their medication prescribed by the clinic’s pharmacy achieved control of their blood pressure in all but six percent of cases. This is a far greater degree of symptom control than is required under the National Health Service targets for doctor’s practices (BMA & NHS Employers 2009). It can be seen from Fig. 2 that the hypertension targets offered maximum reward to doctors who at least measured the blood pressure of 90 percent of patients and control of blood pressure to be in 70 percent of cases.
In the second component of this audit the blood pressure monitoring services were compared using a patient satisfaction questionnaire. As the questionnaire was designed as a component of an ongoing review of blood pressure monitoring at the Medical Centre some of the questions included were used to assist future service development. The practice is planning to install a patient operated automatic blood pressure monitor adjacent to the waiting room. This questionnaire provides a baseline for assessment of changes in patient attitudes after this automated monitor comes into widespread use.
Question 4 – convenient day and time of appointment
An analysis of patient free text comments indicates that there is a preference for morning appointments for blood pressure review. This bias towards morning blood pressure monitoring was greater for the pharmacist-led clinic which at present only offers weekday afternoon or Saturday morning appointments.
Question 5 – length of time waiting to be seen
Patient free text responses showed that patients were more willing to compare waiting to be seen by a Nurse or Pharmacist with waiting times for doctors than they were for Healthcare Assistants. This may reflect a greater respect for the professional status of the former two groups and an unvoiced acceptance of a lower status for the Healthcare Assistants. It should be noted however, that the average rating score given by those seen in the Nurse monitoring clinics was the lowest of the three clinics. The patients seen in the pharmacist-led clinic gave the highest satisfaction ratings.
Question 6 – making you feels at ease
The ability of those monitoring blood pressure to allow their patients to feel at ease is essential if one is to avoid elevated blood pressure readings due to the white coat effect. In the patients’ responses to this question it is clear that the Healthcare Assistants performed less well than the other two clinics. This could be due to a training which focuses on patient monitoring skills in the case of the Nurse clinic. The similar patient satisfaction ratings in the Nurse and Pharmacist clinics demonstrates that during the non-medical prescriber training the pharmacist acquired similar patient monitoring skills to those possessed by the nursing staff.
Question 7 – letting you tell your story
The average rating scores reflect the level of clinical training and involvement in blood pressure treatment at the Medical Centre. Healthcare Assistants appear to have been more focused on the task of obtaining a blood pressure reading than the other two groups. The patients seen in the Nurse clinic appear to have received greater encouragement to discuss their condition when blood pressure was being monitored. Those patients seen by the pharmacist gave on average a higher satisfaction rating score, which might be expected within a prescribing clinic.
Question 8 – satisfaction with appointment
The free text responses to question 8 supported the finding from an averaging of Likert Scale scores that the Healthcare Assistant monitoring was less appreciated than the Nurse clinic and that this was considered inferior to the Pharmacist-led clinic. As for was the case for question 7 the prescribing clinic was associated with greater patient confidence.
Question 11 – how well do you think your medication concerns were listened to?
It was not surprising that the lowest average satisfaction ratings were for the Healthcare Assistants regarding medication concerns as this is not an area of practice they would be expected to offer advice on. The blood pressure monitoring with a Nurse was rated more highly. As there are no non-medical prescribing nurses at the Medical Centre all significant concerns would have required referral to a doctor. In the Pharmacist clinic patients were encouraged to discuss medication concerns and when practical these concerns were addressed by changes to treatment or if this was not possible an explanation as to why it was not considered safe to change the medicine concerned.
Question 12 – were you encouraged to make lifestyle changes?
The average satisfaction ratings for question 12 do not appear to have been supported by the free text responses supplied by the patients. As can be seen in the example responses above there was little evidence of lifestyle advice from either the Healthcare Assistants or the Nurses involved in monitoring patient blood pressures. The patient responses from the pharmacist-led clinic indicated a commitment to improving patient health through lifestyle changes but this was not reflected in the overall satisfaction with lifestyle advice. Due to the different emphasis in nurse and pharmacist training it is not surprising that the pharmacist-led clinic seems to have offered lifestyle advice more frequently. Nurse training is more focused on patient monitoring while pharmacist training has a greater emphasis on medication and promoting healthy lifestyles. The pharmacy involvement in promoting public health is a role recognised in the New Pharmacy Contract (ref).
Question 13 – how well were you involved in medication choice?
The patient responses to questions 13 and 14 have led to an appreciation that these may not have been as useful questions for the survey as had been hoped. Neither the Nurses nor the Healthcare Assistants were particularly involved in medication choice and therefore it is not unreasonable that the patients rated their clinics as less satisfactory in these respects when compared with the prescribing pharmacist clinics.
Question 14 – how would you rate your satisfaction with new medication?
Question 15 – how satisfied are you with your monitoring plan?
The order of patient satisfaction with future monitoring plans for their blood pressure condition followed the same Healthcare Assistant (lowest) then Nurse and Pharmacist (highest average satisfaction rating). Using the free text responses gave good triangulation support for the quantitative assessment as represented by the average rating scores. Healthcare Assistants did not seem to be encouraging regular repeat blood pressure monitoring. In the Nurse-led clinic there were several patients reporting that ongoing monitoring was not applicable but apart from this, patients appear to have been given effective guidance on future blood pressure checks. The patients seen at the pharmacist-led clinic were even more positive in their comments on blood pressure monitoring and this could reflect the pharmacist’s focus on an ongoing monitoring of hypertension. In comparison the other two groups were monitored by those having a greater variety of clinics whereas the pharmacist is only involved with hypertension monitoring and treatment.
Question 16 – how likely are you to recommend the blood pressure clinic you attended?
Question 17 – How likely are you to recommend:
- Doctor (seen face to face)
- Doctor (seen indirectly)
- Pharmacist prescribing to treat raised blood pressure?
Analysis & Conclusion
Quantitative Analysis
The first two groups of patients compared in the clinical audit were selected as a consecutive convenience sample of patients seen in the pharmacist-led hypertension clinic. To minimize any tendency to deliberately select patients for the audit, patients were selected from the start of the year 2009 and all such patients were included who seemed to require an increase in antihypertensive medication to be prescribed within the clinic. Patients who were managed by the medical prescribers, doctors, at the Medical Centre were selected from the clinical system Quality Outcomes Framework database, initially on the basis of matched age and gender to those seen in the pharmacist-led clinic. After initial selection patient’s medication records were examined to ensure that cardiovascular, diabetic and renal history matched as closely as possible within the database.
In the pharmacist-led clinic, there was one patient who was excluded from the Quality Outcomes Framework hypertension target BP5 as being on the maximum medication they could tolerate taking. Examination of the Quality Outcomes Framework found that of the 2348 patients on the hypertension register 68, approximately 2.9 percent, were excluded from the BP5 hypertension target. No patients from the matched group of patients managed by the medical practitioners were excluded from the BP5 target although one patient was advised to start antihypertensive treatment but refused. In the opinion of the researcher, this patient was appropriate for exclusion but that was not considered by the doctor at the time.
When the patient’s blood pressure readings were achieved during the year as compared with their target values as set by the Quality Outcomes framework ninety-two patients seen by the pharmacist achieved target levels. There were a further seven patients for whom treatment failed to reduce blood pressure to the required standard levels. In the matched, the doctor treated, group eighty-five patients were treated to target and in the remaining fifteen patients’ blood pressure remained above target levels.
This can be represented in tabular form as:
These findings can be assessed for statistical dependence by use of the Chi-squared test. This test is used to compare test statistics representing the frequency of occurrence of a categorical variable, in this case, achievement of BP5 blood pressure target. When the frequency of reaching blood pressure targets is compared using the SSPS statistical analysis tool the following results were found.
Pharmacist-led clinic compared to the overall medical center BP5 target proportion.
Chi-squared Test Statistic
While the comparison of the treatment outcomes above does not show statistically significantly increased levels of patient treatment to BP5 targets for both groups, there was an improvement in BP5 achievement in the two groups when compared to the overall results for the Medical Centre. The improvement in both pharmacist and general practitioner treated groups could be due to an exclusion of patients whose blood pressure has not been actively managed during the year. It may be that these patients are those who are less likely to attend the Medical Centre during the normal surgery hours due to work commitments or being housebound.
Fewer patients than expected failed to achieve blood pressure targets in both sample groups. From this, it can be seen that the pharmacist-led clinic is unlikely to be a representative sample of the blood pressure treatment outcomes at the medical center. The probability statistics (Asymp. Sig) is a numerical expression of how often the study samples could be randomly taken from the overall hypertension patient list and demonstrate the same proportion of patients reaching treatment targets.
In the case of those patients treated by the medical practitioners the probability value of 0.297 indicates that almost 30% of random samples would perform as well. This exceeds the probability value of 0.05 which is normally considered to indicate statistical significance in quantitative research. In contrast, the probability value of 0.002 for the pharmacist-led clinic indicates that there is likely to be a significant difference in treatment outcomes between patients seen in that clinic and the overall treatment at the medical center. It can therefore be suggested that the audit found an increased likelihood of achieving target blood pressure levels among those patients seen in the pharmacist-led clinic compared to normal treatment at the Medical Centre.
A comparison of the blood pressure treatment outcomes comparing the cohort from the pharmacist-led clinic and the general practitioner cohort was considered next. In order to make a fair comparison for the audit assessment of hypertension treatment options at the medical center, it is necessary to compare outcomes between the matched patient groups. In choosing these two matched groups of patients there has been a deliberate decision to select only those patients who have been seen during the study period. Frequencies for treatment to target and exceeding target as well as Chi-squared test were performed on ninety-nine patients; one patient had been excluded from the target as being on the maximum tolerated treatment, using SSPS.
Pharmacist clinic patients compared to control cohort treated by general practitioners
- (a) 0 cells (0%) have expected frequencies less than 5. The minimum expected cell frequency is 14.9.
When comparing the pharmacist-led clinic outcomes to the control cohort there was a significant reduction, p < 0.03, in patients failing to achieve Quality Outcomes Framework blood pressure targets.
The pharmacist-led clinic only treated patients in the Medical Centre and the housebound were excluded from the general practitioner group to reduce distorting influences on the audit results. Those seen in the pharmacist-led clinic for workers on Saturday mornings are balanced by patients with a similar profile seen by the Medical Centre’s doctors. It can be seen from Table (ref) that the number of patients excluded from treatment targets is only one for the pharmacist-treated group and none for the doctor-treated group. During the review of hypertensive patient records, it was noticed that there was an increased number of patients excluded from treatment targets if they were housebound and classified as vulnerable patients.
The vulnerable patient’s group have an increased risk of falls which could have life-threatening consequences if a fracture of major bones occurs (ref). The incidence of postural hypotension increases with increased age (ref). A reluctance to risk patient health by increasing blood pressure treatment simply to achieve target blood pressure levels seems clinically justified when most of the medications available for use have the potential to increase postural hypotension (ref). It was a concern that increasing treatment would result in more frequent episodes of hypotension that in discussion with the patient resulted in the exclusion of that patient from the Quality Outcomes Framework on the ground of being on the maximum tolerated treatment.
The audit next compared the medication prescribed to examine differences in prescribing practice. The medication prescribed was compared to the current clinical guidelines for the management of hypertension {NICE, 2006 3 /id}. Due to the general practitioners not qualifying the reasoning behind their medication choices a simple comparison between drug prescribed and stage of hypertension treatment guideline was used as the basis for appropriateness of prescribing. Drug choices were coded as either being to guidelines or not and the frequency of appropriate prescribing was compared between the two cohorts of patients. It was found that 87 of the general practitioner and 97 of the pharmacist prescriber patients were treated to guidelines. The frequency and Chi-squared test findings from the resulting SPSS analysis were as detailed in tables (ref).
Pharmacist-led clinic prescribing compared to standard care cohort
From the SSPS results it can be seen that there were statistically fewer drugs prescribed outside the NICE clinical guidelines in the pharmacist-led clinic. A possible cause for the difference between the two cohorts was that the pharmacist prescriber had previously practiced as a supplementary prescriber and was during this period restricted to prescribing from a clinical management plan.
Qualitative analysis
In the second component of this audit the blood pressure monitoring services were compared using a patient satisfaction questionnaire. As the questionnaire was designed as a component of an ongoing review of blood pressure monitoring at the Medical Centre some of the questions included were used to assist future service development. The practice is planning to install a patient operated automatic blood pressure monitor adjacent to the waiting room. This questionnaire provides a baseline for assessment of changes in patient attitudes after this automated monitor comes into widespread use.
There were two sections to the patient satisfaction questionnaire. In the first section questions related to patient demographics, appointment arrangements and satisfaction with consultation skills. Patients were allowed to select one option from six ratings from ‘poor to fair’ to ‘excellent’. The decision to have a six point evaluation was deliberate to avoid a centre position tendency, therefore enforcing an above or below midpoint satisfaction rating. It was assumed that performance that did not achieve at least a ‘poor to fair’ rating would result in a complaint to the Medical Centre. During the period of the study there were no patient complaints received about the blood pressure monitoring services. Patient responses were scored according to the following grid.
The second section sought patient attitudes to the alternative prescribing services offered at the Medical Centre. Patients were asked how likely they were to recommend face to face consultation with a doctor, remote doctor prescribing and the pharmacist-led hypertension clinic. Remote doctor prescribing reflects the normal process when a nurse who does not have non-medical prescribing qualification monitors the patient and interrupts a doctor between consultations for a prescription. It is difficult to identify the prescriber when remote prescribing by doctors is practiced as depending on the doctor-nurse relationship the decision of which drug to use could be made by either healthcare professional. This is a continuation of the situation before the introduction of non-medical prescribing where a specialist nurse would write prescriptions for a doctor to sign.
Patient demographics from the questionnaire survey
Cross tabulation of the patient questionnaire responses for each of the blood pressure monitoring clinics found the following.
Patient gender distribution across monitoring clinics
The increased representation of female respondents in the nurse clinic was due to the inclusion of blood pressure checks for those patients who take oral contraceptive treatment in their monitoring clinic. This was also evident in the age groups identified in the next question.
Patient age distribution across monitoring clinics
The age of patients seen in different monitoring clinics reflects the differing roles of those conducting the clinics. As seen previously, the nurse clinic examined oral contraceptive patients while the healthcare assistant and pharmacist clinics more frequently saw older patients. The bias towards older patients was as expected since hypertension is a condition with increasing incidence as age increases (ref). Reduced numbers above the age of 90 years reflects the overall patient demographics at the Medical Centre.
Responses to question 4 were considered to be more appropriate to service planning within the Medical Centre and will not be considered as part of this study. However, there was an overall satisfaction with 98.3% (175) of responses indicating appointments were convenient.
Satisfaction with time waiting to be seen in the different clinics was examined in question 5
The statistical differences shown were calculated using SSPS to compare the means values between the clinic referred to and the pharmacist-led clinic. The average satisfaction rating was significantly higher for the pharmacist-led hypertension clinic and these findings were confirmed by triangulation with the free text responses from the 114 patients who replied.
To avoid excess presentation of tabulated data the responses to questions 6 to 15 are listed with significant t-test statistics from SSPS when applicable.
Average response ratings and significant SPSS findings for questions 6 to 15
For all questions the pharmacist average satisfaction rating exceeded that of the other clinic services. The difference between clinics ratings for questions 6 to 15 was only statistically significant when comparing the healthcare assistant ratings to the pharmacist-led clinic. Full cross tabulation results from questionnaire analysis is presented in appendix 2, (to be added) free text responses were used to triangulate the findings for the above questions and a high degree of confirmation was found.
In the second section a different scoring grid was deliberately chosen to use a five category rating system. The possibility of a neutral position was to allow respondents the option to register an unwillingness to recommend the different prescribing options available at the Medical Centre. Scores were allocated to patient responses for questions 16 and 17a to 17c according to the following grid.
Patients average ratings on willingness to recommend services in response to questions 16 to 17c and t-test statistics where significant were found between pharmacist-led clinic and alternative clinics:
Comparison with free text boxes for triangulation confirmed the findings above. The reduction in endorsement of doctor prescribing options by patients seen in the pharmacist-led clinic was matched by and increased endorsement of pharmacist prescribing. Patients who had not experienced the pharmacist hypertension clinic were less likely to recommend that option demonstrating that a lack of exposure to non-medical prescribing is common at the Medical Centre. This further supports the findings from Scotland where it was found that exposure to pharmacist prescribing increased patients’ acceptance of this new area of practice (Stewart et al. 2008).
Key Results from the Study
A patient satisfaction survey was performed during 2008 to ascertain patients views of the pharmacist prescriber’s consultation skills. The questionnaires were based on an approval scale system offering assessment options of very poor, poor, fair, good, very good, excellent or does not apply (Likert 1932). The traditional Likert scale has been modified to force either an approval or disapproval and therefore avoid the possibility of unclear attitudes being recorded. The table showing the topics for which opinions were sought are shown in Fig. 8.
Figure 6: Likert scale patient satisfaction survey for pharmacist-led hypertension clinic
The results from this survey were highly supportive of the pharmacist-led clinic. There were three patient rating responses which indicated that they did not consider that the question applied to their experience. One patient rated their time spent in the clinic as good, but all responses were in the ‘very good’ or ‘excellent’ categories. It can be seen from the patient satisfaction survey results that there was generally a high level of satisfaction with the patient consultation skills of the pharmacist prescriber.
As ninety four per cent of patients seen in the pharmacist-led hypertension clinic achieved target blood pressure levels it can be seen that those treated in the clinic exceeded the proportion of patients with controlled blood pressure set by the National Health Service (BMA & NHS Employers 2009). This improvement in hypertension control has also been shown in other pharmacist-led clinics in the United Kingdom (Reid et al. 2005). In a foreign study the positive influence of pharmacist involvement in a hypertension clinic has been shown with particular emphasis on adherence with prescribed medication and lifestyle changes, particularly relating to exercise (Sookaneknun et al. 2004). Therefore it should be expected that the management of hypertension by a pharmacist prescriber would achieve a high level of symptom control. The Published evidence from the United States of America supports the ability of pharmacists to manage hypertension patients as effectively as physicians (Okamoto and Nakashiro 2001). In this study it was found that patient satisfaction was higher than the physician-managed hypertension group and while no such claims are made for the Highcliffe Medical Centre pharmacist-led clinic high levels of patient satisfaction were reported. The American study concluded that pharmacists management of hypertension patients can be a cost-effective alternative to physicians and this is should encourage a widespread adoption of pharmacist prescribing hypertension clinics. The pharmacist prescriber saw three hundred and forty of the patients on the hypertension register at the Highcliffe Medical Centre. It is not practical to see all the hypertension patients in the pharmacist-led clinic due to a proportion of these people requiring home visits or being managed in another clinic, for example the clinic for patients with confirmed diabetes. However, if the hypertension clinic was run on a daily basis during the week the pharmacist could manage over a half of the hypertension register patients.
After analyzing the results of the study, it can be suggested that the community pharmacists should all develop their professional skills further by spending a portion of their working week as part of the primary care team prescribing in a multidisciplinary team environment. As far as generalization was concerned, the case study highlights that potentially any well motivated community pharmacist could successfully perform an independent prescribing role in a GP practice. This would allow the integration of community pharmacy into the primary care team thus terminating its present isolation as a mixed economy ‘business’ of healthcare outsiders.
References
Anon 2008, Change 4 life, UK, Department of Health, Ref Type: Pamphlet.
Barber, N Batty, R & Ridout, D 1997, ‘Predicting the rate of physician-accepted interventions by hospital pharmacists in the United Kingdom’, Am J Health Syst.Pharm, vol. 54, pp. 397-405.
Barber, N Rawlins, M & Frankin, B 2003, ‘Reducing prescribing error: Competence, control and culture’, Quality and Safety in Health Care, vol. 12, pp. 29-32.
Berlowitz, DR Ash, AS Hickey, EC Glickman, M Friedman, R & Kader, B 2003, ‘Hypertension Management in Patients With Diabetes: The need for more aggressive therapy’, Diabetic Care, vol. 26 no. 2, pp. 355-359.
BMA & NHS Employers 2009, Quality and Outcomes Framework guidance for GMS contract 2009/10, BMA & NHS Employers, London.
Bpassoc 2009, UK high blood pressure rises, but diagnoses increase faster, Web.
Callum, K Carr, N & Gray, A 2010, The 2002 report of the national confidential enquiry into preoperative deaths, National Confidential Enquiry into Preoperative Deaths, London.
Casigia, E & Palatini, P 1998, ‘Cardiovascular risk factors in the elderly’, J Hum Hypertension, vol. 12, pp. 575-581.
Centre for the Advancement of Inter-professional Education 2000, Principles of inter-professional education, McGraw Hill, London.
Cooper, RJ Anderson, CAT Bissell, P Guillaume, L Hutchinson, A James, V Lymn, J McIntosh, A Murphy, E Ratcliffe, J Read, S & Ward, P 2008a, ‘Nurse and pharmacist supplementary prescribing in the UK – a thematic review of the literature’, Health Policy, vol. 85, pp. 277-292.
Cooper, RJ Anderson, C Avery, T Bissell, P Guillaume, L Hutchinson, A Lymn, J Murphy, E Ratcliffe, J & Ward, P 2008b ‘Stakeholders’ views of UK nurse and pharmacist supplementary prescribing’, J Health Serv Res Policy, vol. 13 no. 4, pp. 215-221.
Cooper, RJ Anderson, C Avery, T Bissell, P Guillaume, L Hutchinson, A James, V Lymn, J McIntosh, A Murphy, E Ratcliffe, J Read, S & Ward, P 2008c, ‘Nurse and pharmacist supplementary prescribing in the UK–a thematic review of the literature’, Health Policy, vol. 85 no. 3, pp. 277-292.
Cooper, RJ Lymn, J Anderson, C Avery, A Bissell, P Guillaume, L Hutchinson, A Murphy, E Ratcliffe, J & Ward, P 2008d, ‘Learning to prescribe – pharmacists’ experiences of supplementary prescribing training in England’, BMC Med Educ., vol. 8, pp. 57.
Courtenay, M Carey, N & Burke, J 2007, ‘Independent extended supplementary nurse prescribers, their prescribing practice and confidence to educate and assess prescribing students’, Nurse Educ.Today, vol. 27 no. 7, pp. 729-747.
Cranney, M Barton, S & Walley, T 1998, ‘The management of hypertension in the elderly by general practitioners in Merseyside: the rule of halves revisited’, British J General Practice, vol. 48, pp. 1146.
Dean, B Schachter, M & Vincent, C 2002, ‘Prescribing errors in hospital inpatients: their incidence and clinical significance’, Quality and Safety in Health Care, vol. 11, pp. 340 – 344.
Department of Health 1968, Medicines Act 1968, Ref Type: Statute.
Department of Health 1999a, Final Report of the Review of Prescribing, Supply and Administration of Medicines, Department of Health, London.
Department of Health 2005, Implementing the new Community Pharmacy Contractual Framework – information for PCTs, Web.
Department of Health 1999b, Final Report of the Review of Prescribing, Supply and Administration of Medicines, Department of Health, London.
Department of Health 2008, Making the Connections: Using healthcare professionals to deliver organisational improvements, Department of Health, London.
Department of Health 2011, Pharmaceutical Services (Advanced and Enhanced Services), Directions, London.
Duggan, S Ford, GA & Eccles, M 1997, ‘Doctors’ attitudes towards the detection and treatment of hypertension in older people’, J Hum Hypertens, vol. 11 no. 5, pp. 271-276.
Elston, A 1996, “Professional Socialisation” In Key Concepts in Medical Sociology, Sage Publications, London.
Emmerton, L Marriott, J Nissen, L & Dean, L 2005, ‘Pharmacists and prescribing rights: review of international developments’, J Pharmacy and Pharmaceutical Sciences, vol. 8 no. 2, pp. 217-225.
Fahey, T & Lancaster, T 1995, ‘The detection and management of hypertension in the elderly of Northamptonshire’, J Public Health, vol. 17 no. 1, pp. 57-62.
Gatewood, SB Stanley, DD Goode, JV 2003, ‘Implementation of a comprehensive pre-travel health program in a supermarket chain pharmacy’, J Am Pharm Assoc, vol. 49, pp. 660-669.
George, J McCaig, D Bond, C Cunningham, I Diack, H & Stewart, D 2007, ‘Benefits and challenges of prescribing training and implementation: Perceptions and early experiences of RPSGB prescribers’, Int.J Pharm Pract., vol. 15, pp. 23-30.
George, J McCaig, DJ Bond, CM Cunningham, IT Diack, HL Watson, AM & Stewart, DC 2006, ‘Supplementary prescribing: early experiences of pharmacists in Great Britain’, Ann Pharmacother, vol. 40 no. 10, pp. 1843-1850.
Guidelines Committee 2003, ‘2003 European Society of Hypertension – European Society of Cardiology guideline for the management of arterial hypertension’, Journal of Hypertension, vol. 21, pp. 1011-105.
Gu, Q Paulose-Rain, R Dillon, C & Bart, V 2006, ‘Antihypertensive drug use among US adults with hypertension’, Circulation, vol. 113, pp. 213-221.
Hanninen, T & Soininen, H 1997, ‘Age-associated memory impairment. Normal aging or warning of dementia?’, Drug Aging, vol. 11 no. 6, pp. 480-489.
Hepler, CD & Strand, LM 1990, ‘Opportunities and responsibilities in pharmaceutical care’, American Journal of Hospital Pharmacy, vol. 47, pp. 533-543.
Herbert, C Wright, J Maclure, M Wakefield, J Dormuth, C Brett-Maclean, P Legare, J & Premi, J 2004, ‘Better prescribing project: a randomised controlled trial of the impact of case-based educational modules and personal prescribing feedback on prescribing for hypertension in primary care’, Fam. Pract., vol. 21, pp. 575-581.
Hess, KM 2010, ‘Measuring outcomes of a pharmacist-run travel clinic located in an independent community pharmacy’, J Am Pharm Assoc, vol. 50, pp. 174-180.
Horrocks, S Anderson, E & Salisbury, C 2002, ‘Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors’, BMJ, vol. 324, pp. 819-823.
HOT Study Group 1998, ‘Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: Principal results of the Hypertension Optimal Treatment (HOT) randomised trial’, Lancet, vol. 351 no. 9118, pp. 1755-1762.
Hind, CAM Bond, CM Lee, AJ & Teijingeb ER 2008, ‘Needs Assessment Study for Community Pharmacy Travel Medicine Services’, Journal of Travel Medicine, vol. 15 no. 5, pp. 328–334.
Hughes, CM & McCann, S 2003, ‘Perceived professional barriers between community pharmacists and GPs: A qualitative assessment’, Br J Gen Pract, vol. 53, pp. 600-606.
Hyre, AD Krousel-Wood, MA Muntner, P Kawasaki, L & DeSalvo, KB 2007, ‘Prevalence and predictors of poor antihypertensive medication adherence in an urban health clinic setting’, J Clin Hypertens (Greenwich), vol. 9 no. 3, pp. 179-186.
Jones, R John, D & Luscombe, D 2007, ‘An exploratory qualitative study of the views of UK pharmacists undertaking training in supplementary prescribing’, J Appl Ther Res, vol. 6 no. 2, pp. 32-40.
Kotchen, T 2006, ‘From Clinical Trials to Clinical Practice: Why the Gap?’, Hypertension, vol. 48, pp. 196-197.
Laurant, MGH Hermens, RPMG Braspenning, JCC Sibbald, B & Grol, RPTM 2004, ‘Impact of nurse practitioners on workload of general practitioners: randomised controlled trial’, BMJ, vol. 328 no. 7445, pp. 927.
Likert, R 1932, ‘A Technique for the Measurement of Attitudes’, Archives of Psychology, vol. 140, pp. 1-55.
Laurance, J 2008, ‘Beta blockers cost more lives than they save, study claims’, The Independent on Sunday.
Lloyd, F & Hughes, CM 2007, ‘Pharmacists’ and mentors’ views on the introduction of pharmacist supplementary prescribing: A qualitative evaluation of views and context’, Int. J Pharm Pract., vol. 15, pp. 31-37.
Loveman, E Royle, P & Waugh, N 2003, Specialist nurses in diabetes mellitus, Cochrane Database Syst Rev: CDoo3286.
Menard, J & Chatellier, G 1995, ‘Limiting factors in the control of BP: Why is there a gap between theory and practice?’, J Hum Hypertens, vol. 9, pp. S19-S23.
Mikeal, RL Brown, TP Lazarus, HL & Vinson, MC 1975, ‘Quality of pharmaceutical care in hospitals’, Am J Hosp Pharm, vol. 32, pp. 567-574.
National Collaborating Centre for Chronic Conditions 2008, Chronic Kidney Disease: National clinical guideline for early identification and management in adults in primary and secondary care, Royal College of Physicians, London.
NICE Clinical Guideline 2004, Hypertension: Management in adults in primary care: Pharmacological update, Royal College of Physicians, London.
Nuffield Foundation 1986, Pharmacy: The report of a committee of inquiry appointed by the Nuffield Foundation, The Nuffield Foundation, London.
OFT 2007, The Pharmaceutical Price Regulation Scheme, Web.
Okamoto, MP & Nakashiro, RK 2001, ‘Pharmacoeconomic Evaluation of a Pharmacist-Managed Hypertension Clinic’, Pharmacotherapy, vol. 21 no. 11, pp. 1337-1344.
Parkin, B 1999, ‘Pharmacy in a new age: The road to the future’, Tomorrow’s Pharmacist, pp. 58-60.
Primatesta, P Brookes, M & Poulter, NR 2001, ‘Improved hypertension management and control: Results from the health survey for England 1998’, Hypertension, vol. 38 no. 4, pp. 827-832.
Robinson, KR 2000, ‘Nurse-managed primary care delivery clinics’, Nurse Clin North Am, vol. 35 no. 2, pp. 471-479.
Reid, F Murray, P & Storrie, M 2005, ‘Implementation of a Pharmacist-Led Clinic for Hypertensive Patients in Primary Care – A Pilot Study’, Pharmacy World and Science, vol. 27 no. 3, pp. 202-207.
Safar, ME 2005, ‘Systolic hypertension in the elderly: Arterial wall mechanical properties and the renin-angiotensin-aldosterone system’, J Hypertension, vol. 23 no. 4, pp. 673-681.
Scottish Intercollegiate Guidelines Network 2001, ‘Hypertension in Older People’, National Clinical Guideline, pp. 1-50.
Schroeder, C.A Trehearne, B & Ward, D 2000, ‘Expanded role of nursing in ambulatory managed care. Part II: Impact on outcomes of costs, quality, provider and patient satisfaction’, Nurs Econ, vol. 18 no. 2, pp. 71-78.
Sherman, FT 2009, ‘Opinion: Treat hypertension in the elderly. Set a goal, start low, go slow, and try to get to goal!’, Geriatrics, vol. 64 no. 10.
Siegel, D Lopez, J Meier, J Goldstein, MK Lee, S Brazill, BJ & Matalka, MS 2003, Academic detailing to improve antihypertensive prescribing patterns, Web.
Sookaneknun, P Richards, RME Sanguansermsri, J & Teerasut, C 2004, ‘Pharmacist Involvement in Primary Care Improves Patient Clinical Outcomes’, The Annals of Pharmacotherapy, vol. 38 no. 12, pp. 2023-2028.
Soumerai, SB McLaughlin, TJ & Avorn, J 1989, ‘Improving drug prescribing in primary care: a critical analysis of the experimental literature’, The Milbank Quarterly, vol. 67 no. 2, pp. 268-317.
Staessen, JA Faggard, R 1997, ‘The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators 1997. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension’, Lancet, vol. 350, pp. 757-764.
Stafford, RS Monti, V Furberg, CD & Ma, J 2006, ‘Long-term and short-term changes in antihypertensive prescribing by office-based physicians in the United States’, Hypertension, vol. 48 no. 2, pp. 213-218.
Stewart, D 2010, Exploring and Evaluating Pharmacist Prescribing, School of Pharmacy & Life Sciences, Robert Gordon University, Aberdeen.
Stewart, DC George, J Bond, CM Cunningham, IT Diack, HL & McCaig, DJ 2008, ‘Exploring patients’ perspectives of pharmacist supplementary prescribing in Scotland’, Pharm World Sci., vol. 30 no. 6, pp. 892-897.
The Audit Commission 2002, A spoonful of sugar: medicines management in NHS hospitals, The Audit Commission, London.
The ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group 2002, ‘Major outcomes in high-risk hypertensive patients randomised to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)’, JAMA, vol. 288, pp. 2981-2997.
Twinn, S Lee, A Lam, AT Thompson, DR Cheng, F & Goggins, W 2010, ‘Effectiveness of different models of health care delivery in the primary care setting of general outpatient clinics in Hong Kong’, Hong Kong Med J, vol. 16 no. 3, pp. 8-12.
Warchal, S Brown, D Tomlin, M & Portlock, J 2006, ‘Attitudes of successful candidates of supplementary prescribing courses to their training and their extended roles’, Pharmaceutical Journal, vol. 276, pp. 348-352.
Weiss, MC Sutton, J & Adams, C 2006, Exploring innovations in pharmacy practice: A qualitative evaluation of supplementary prescribing by pharmacists, The Royal Pharmaceutical Society of Great Britain, London.
WHO/ISH Writing Group 2003, ‘World Health Organisation (WHO) / International Society of Hypertension (ISH) statement on management of hypertension’, J Hypertension, vol. 21 no. 11, pp. 1983-1992.
William, B Poulter, NR Brown, MJ Davis, M McInnes, GT Potter, JF Sever, PS & Thom, SM 2004, ‘British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): Summary’, BMJ, vol. 328, pp. 634-640.
Yusuf, S & Sleight, PJ 2003, ‘Effects of an angiotensin-converting enzyme inhibitor, ramipril, on cardiovascular risk in high-risk patients’, N Eng J Med, vol. 342 no. 3, pp. 145-153.
Appendix 2