Introduction
Anxiety is an adaptive response of the human brain to stimuli that is perceived to be of danger to the individual. It is a vital protective response that develops early in life usually during infancy. Under normal circumstances, its main aim is to protect or warn an individual of possible harm or impeding danger. An example is the fear that a child expresses in the threat of being dropped from an adult’s arms or fear of the dark. An anxiety disorder follows a defined developmental blueprint that has a lasting deleterious effect on the affected child.
Anxiety may range from a mild form to very severe form depending on the individual and stimuli precipitating the anxiety. Anxiety in itself is meant to warn and protect the organism, however, in some cases it becomes pathological posing a danger to the organism. At such times it occurs regularly and worsens with each episode leading to development of acute evasive behavior (Pine et al., 2009).
Anxiety occurs at any age and is termed pathological when its occurrence becomes frequent, severe and takes a physical toll on the individual. Diagnosis of anxiety in children is complex since as children grow up they express anxiety and a wide range of fears as normal developmental phenomena. Children show a variety of emotions that can be misinterpreted as anxiety. The outward manifestation of anxiety is mediated by the autonomic nervous system and is manifested as excessive incapacitating state of worry. With time this state takes a toll on social and developmental aspects of the child. As such it interferes with normal day-to-day activities of the child. At this time the anxiety disorder becomes pathological and requires urgent initiation of appropriate interventions (Schniering, Hudson & Rapee, 2000).
Of the childhood psychiatric disorders, anxiety disorders are the most prevalent accounting for 5-18% of all childhood psychiatric conditions (Steinhausen, Metzke, Meier & Kannenberg, 1998). Studies show a strong correlation between occurrence of anxiety at a young age and full blown development of severe anxiety disorders in adolescence and young adulthood. Anxiety disorders are of a big concern both to the health community and public in general since they have a big social impact on children affected and their immediate family. Anxiety disorders interfere with normal day to day activities such as attendance of school, decreased sociability of the affected child and in essence results in tensions within the family that may grow into societal conflicts (Langley, Bergman, Mccracken & Piacentinni, 2004). Of the anxiety disorders, specific phobias and separation anxiety disorders manifest earliest in developing children.
Diagnosis of anxiety disorders is a complex issue due to tendency of overlap of several anxiety disorders and occurrence of co-morbid states in children with anxiety disorders. To improve diagnosis, systematic diagnostic criteria were developed. These criteria are the Diagnostic and Statistical Manual of Mental Disorders (DSM) and the International Classification of Diseases (ICD). These diagnostic criteria are not wholesome in addressing anxiety disorders in children hence they have been modified to try and include unique disorders that manifest in children. Based on the DSM criteria, anxiety disorders are classified in four major categories with numerous sub categories. Failure to properly diagnose these conditions has serious and long stretching effects to the individual and society. Furthermore, choice of intervention becomes problematic, since health care providers must choose between the two major approaches of management and this has an impact on the child. The major disorders are generalized anxiety disorder, panic disorder, obsessive compulsive-obsessive disorder, phobic disorder and dissociative disorder.
Management of anxiety disorders encompasses either pharmacological or non-pharmacological approaches or a combination of both methods. Studies have demonstrated increased success rate when both methods are employed in management of some forms of anxiety disorder (Abramowitz, 1997).
Anxiety in Children
About 18% of all psychiatric conditions manifest in children. It has been shown that a young age is a core factor for advancement of anxiety disorders. These disorders have a wide continuum varying from mild unnoticeable cases to severe incapacitating and life threatening cases. Diagnosis of anxiety disorders has proved to be a headache since in most cases children tend to be treated as “small adults” and management follows the same criterion (Briggs-Gowan, 2003).
Pathological anxiety in children manifests as prolonged sessions of evasive behavior that finally results in impairment of day to day activities and deviant behavior in affected children. Sometimes, in diagnosing anxiety, there is no clear line between ordinary fears and full blown anxiety since as children grow up they manifest a myriad of fears that may be confused with anxiety disorders (Muris, Merckelbach, Mayer & Meesters).
Occurrence of these innumerable fears has been a major hindrance in proper diagnosis and subsequent management of anxiety and anxiety disorders in children. Anxiety sometimes has a slow sub-clinical manifestation without any obvious phenotypic manifestations and goes unnoticed and hence misdiagnosed (Bell-Dollan, Last & Strauss, 1990). Of importance is the inability of young children to articulately express themselves to the clinician since they lack proper cognitive character of expressing their emotions and due to their ambiguousness in explaining what and how they feel making it difficult to employ the diagnostic methodologies in assessing the severity and type of anxiety disorder manifested.
Further studies have demonstrated that anxiety conditions in children are “unwavering” such that they will always manifest themselves as the child grows unless proper and timely interventions are initiated (Briggs-Gowan et al., 2003). Anxiety disorders take a toll on the child’s life and significantly interfere with the quality of life of the affected child.
Anxiety in children manifests itself very early in a child’s life, as early as a few weeks after birth. As children grow they are subject to encounter what is termed as “dangerous” situations such as when they are left alone by their mothers. They respond to these situations through fear manifested as anxiety. The body prepares the child for imminent danger as a protective mechanism whereas on the outside this is viewed as anxiety. Failure to address these conditions at early age may lead to progression into a chronic form of anxiety.
A wide variety of social demographic factors influence development of anxiety in children. Studies have shown a high incidence of separation anxiety disorder in children of European descent as compared to those of African American descent irrespective of age and gender. In contrast African American children tend to show more of separation anxiety as compared to their European American counterparts (Last, 1993).
Poverty is a core factor that influences development of anxiety disorders in children. It has been demonstrated that the higher the poverty indices, the higher the probability of occurrence of a given type of anxiety disorder. Gender also plays a major role in specific forms of anxiety. Studies have shown that female children tend to have high incidences of certain phobias such as blood phobia as compared to male children of the same age (Costello, Egger & Angold, 2005).
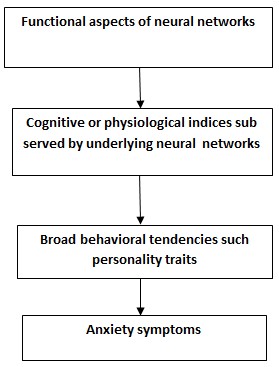
No single factor that brings about anxiety has been elucidated so far. Instead it is believed that anxiety disorders are a product of several factors both somatic and psychosocial. They are a myriad of factors that are either independent or dependent of each other. These features include anxiety disorders attributed to a genetic predisposition that renders children to a high tendency to develop and manifest anxiety. In addition, a psychological factor that renders children to increased susceptibility to anxiety and anxiety related conditions with perception of impeding threat or danger to the child’s life has been proposed. The last of the factors encompasses all the things a child encounters as he or she grows up, as such one responds to these circumstances by developing specific anxiety disorders as a defensive mechanism to them. All these factors have been termed as the “triple-vulnerability” model of progression of anxiety (Barlow, 2000).
Genetic factors have been shown to predispose individuals to certain anxiety disorders. Studies carried out in twins show evidence of genetic factors in some forms of anxiety. Apart from genes implicated in causation of general anxiety disorders, similar genes have been demonstrated in children with depressive symptoms. Furthermore there is a broad familial component in relation with anxiety disorders. (Keandler, Neale, Kessler, Keath, & Heaves, 1993).
The personality of a child also plays a role in progression of anxiety disorders. Personality denotes a trait in behavior of a child. Personality is elaborated through a trait called “behavioral inhibition” which determines a child’s extent of sociability. Those children with high “behavioral inhibition” tend to be prone to development of anxiety disorders. Furthermore, those children whose parents have high “behavioral inhibition” had a higher tendency to develop anxiety disorders especially phobias such as agoraphobia (Kagan et al., 1988).
Separation Anxiety Disorder
Separation Anxiety Disorder (SAD) has the highest prevalence of the childhood anxiety disorders, with female children having a greater percentage when compared to male children. Separation anxiety under normal circumstances is a protective mechanism devised by the child to keep it close to its care taker. Cognitive-behavioral approach has proved to be effective in management of such a disorder (Weems & Carrion, 2003)
SAD has been retained in the latest edition of American Psychiatric Nomenclature. It was first described in DSM-III in the chapter of childhood disorders in DSM-IV. The major feature of this disorder is the fear of being detached from key elements to which the child is attached such as home or relatives whom the child is dependent on and used to. The children are anxiously pre-occupied by thoughts that their parents may be involved in accidents or face a calamity while on the other hand; some suffer from fear of being kidnapped. Nightmares also occur which may persist into adolescence (Bell-Dolan & Brazeal, 1993).
Fear is immense and inconsistent with the normal separation anxiety experienced around six months to six years of childhood. Avoidance behaviors characteristic to this disorder are informally classified according to the severity of the features. Mild symptoms may include the urge to always communicate with parents through phone while at school or delay in leaving home for school.The child may feel uncomfortable with schedules noticeably through constant queries about them.
Moderate degree can be noticed through resistance of the children to participate in activities that will leave them detached from their parents for a few hours such as sleep over while small children tend to cling to their parents wherever they go. The severe form is epitomized by refusal to go to school, declining to sleep in their separate rooms and clinging behavior in every activity that their patrons engage in. They may desperately forge excuses in order to escape group activities like camps just to be unified with their parents. This may involve risky behavior such as walking away albeit in the presence of supervision. Further research has ruled out suicidal tendencies in such children (Krohne & Hock, 1991).
Progression from the mild degree to severe form is gradual. It may start with minor complaints followed by claims of experiencing nightmares gradually descending into sleeping with their parents. Furthermore, the children may procrastinate going to or absconding school. The climax is characterized by clinging and crying behavior in the advent of separation. The physical aspect evolves from minor complains like stomach ache to major concerns such as panic attacks or emesis in the event of separation. This pattern noticeably occurs during weekdays (Livingston, Taylor & Crawford, 1988).
SAD is diagnosed by persistence of a minimum of four of the above features for a period more than one month with the onset before eighteen years of age during the pre-puberty period (Bowen, Offord & Boyle, 1990).This must be in tandem with clinical diagnosis of significant distress or impaired functioning in aspects of life like learning and social aspects such as forging or keeping friendships.
Expression of the different features has been studied and found to be dependent on the age with younger children reporting more features than older ones. Five to eight year olds commonly experienced nightmares, declined attending school and had the fear of calamity befalling those they are attached to. Nine to twelve year olds were more likely to exhibit severe distress at the time of separation while adolescents (age thirteen to sixteen) generally reported somatic features and declining to attend school. SAD has a high index of recovery in most children although some studies demonstrate an elevated risk of development of other anxiety disorders (Kendall, Hedtke & Aschenbrand, 2006).
Social Anxiety Disorder
Social anxiety disorder previously called social phobia, occurs in the society at a significant rate. It is essentially characterized in DSM-IV by immense and persistent fear when one experiences a social encounter including exposure to peculiar people or situations in which one is required to perform. The person reacts anxiously to the situation which may manifest in the form of panic attacks. Furthermore, the child develops evasive behavior to reduce the effects associated with this anxiety disorder. In children and adolescents, limited cognitive development makes them fail to realize that the fear is great and unwarranted. Diagnosis is made when the symptoms persist for more than six months (Kearney & Albano, 2007).
In DSM-IV, this disorder is classified into generalized and non-generalized forms. In generalized forms, fear encompasses most of the social situations and generally occurs earlier than the non-generalized forms. Hence studies have shown that this is the most common form in children and adolescents. There is also increased risk of suffering from co-morbid psychiatric disorders and early temperament inhibition (Velting & Albano, 2001). In both forms, victims generally have fewer friends, feel lonely and are reluctant to participate in group activities..Avoidance behavior occurs both in group activities or family set up with individuals needing persuasion to participate in group activities. The adolescents experience difficulties in dating and job seeking. In summary, the children fear being embarrassed, negatively evaluated and rejected (Staub, Tursky & Schwartz, 1971).
Social phobia is not common in early childhood as it is in adolescents. Physical manifestations such as stomach ache accompany the fear early on, with trembling while addressing an audience, with blushing and sweating occurring in adults. This tends to suppress the social skills of these children (Cobham, Dadds & Spence, 1997).
Obsessive Compulsive Behavior
Abbreviated as OCD, mainly occurs when the child is pre-occupied by recurring obsessions accompanied by compulsions for more than one hour per day (American Psychiatric Association, 1994). Studies have established the average age of commencement of obsessive-compulsive disorder is from ten to twelve years (Leonard & Rapoport, 1991). According to the DSM-IV criteria, features in adults are similar to those in children and involve repetition of activities in daily life aimed at achieving perfection. This averagely occurs at the age of ten to twelve and a half years. The study also showed early onset in male subjects as compared to their female counterparts, with signs manifesting as early as seven years in male children. Parents of these children have reported that the pattern of obsessions constantly changes with time, which is uncharacteristic with non-anxious children. Amongst the main behaviors that characterize OCD was clinging rituals accounting for more than 85% of reported cases (Swedo, Rapport, Leonard, Lenane & Cheslow, 1989).These individuals repeat the same pattern of hand washing on a daily basis. Other behaviors include compulsion to ensure that things are in the order that they deem right, over expressed distressing thoughts with the aim of preventing feared events which are generally unrealistic and the fear of being morally unclean. However this should not be confused with features that occur as a result of physiological response to use of a chemical or drug substance or an underlying medical condition.
It is worth noting that the tendency to arrange things in a specific order is part of normal development of all children before nine years of age. However, this behavior tends to disappear afterwards. Children with anxiety disorders exhibit excessive anguish when the order of things is interrupted or stopped.OCD is noticed by parents when the habits eventually interfere with the performance of the family activities. They tend to be slow in arranging personal items and perform repetitive non-sensical behavior like tapping on food prior to eating.
According to an investigation carried out fifty to sixty percent of OCD diagnosed children have experienced major global functioning impairment with inability to accomplish tasks within the stipulated time frame (Freeman, Garcia, Coyne, Leonard & Compton, 2007).Those with explicit nighttime rituals find inviting friends for sleep over and vice versa challenging. There is increasing complexity of performing tasks like doing homework due to repetitive checking in a bid to achieve perfection. Over-dependence on the family is shown when adolescents are unable to cope with activities that require autonomy from the family such as dating or picnics with peers. This occurs because independence provokes excessive anxiety which is overwhelming to handle.
Onset occurs earlier in males than in females. Studies have shown that females present more with compulsion symptoms while males tend to feature more obsessive symptoms. Early manifestation of OCD may be associated with depression and an increased risk of developing other anxiety disorders like SAD later on in life. In addition mood disorders are more prevalent.Tourette’s disorder increases the incidence of OCD by thirty five to fifty percent though the incidence of this disorder is low in OCD with occurrence of about five to seven percent (Geller et al., 2001).
Specific Phobias
This refers to excessive fear upon exposure to restraining objects or situations.This stimulus triggers anxiousness in the individual which may present as panic attacks. As with the other anxiety disorders, this triggers avoidance or endurance of the stress without realizing that this reaction is excessive especially in children. The reaction is excessive in relation to situational demands and may interfere with the individual’s schedules or routine.
This condition tends to manifest itself independent of the other anxiety disorders and involve fear of situation related incidents or objects especially those threatening personal safety such as heights, being in the dark alone, some animalis like dogs and very loud noises. Anticipation of events may also be exhibited. This response is portrayed in all the three components of anxiety which are; physiological, behavioral and cognitive functions thus it is important to isolate the major precipitating factor for the response in order to accurately diagnose and subsequently draw a treatment plan.
The nature of the avoidance behavior is related to the magnitude of fear and the extent to which functioning is interfered (Esau, Conradt & Petermann, 2000). Physiological symptoms that present with the panic attacks include: increased pulse rate, sweating profusely, increased breathing rate, trembling and stomach aches. The specific fears tend to appear at different ages over the lifespan of an individual, with one retrospective study showing that the fear of animals tends to start at seven years, the fear of blood at nine years of age respectively. This peaks in a period between ten and thirteen years of age.
Parents generally notice the need to take the child for treatment when the fear interrupts with smooth functioning of the family. In most cases, the trigger can be avoided but severe response may lead to aggression from the child. Some children present with vasovagal fainting reaction upon administration of injections. According to the study, over seventy to seventy five percent of social phobia victims were affected. Characteristically this reaction starts with transient hyperventilation followed by decrease in heart rate with eventual decrease in arterial and venal blood pressure. Severe distress may cause the children to be ridiculed by their peers.
Generalized Anxiety Disorder
This disorder mainly presents with irrepressible fear and worrying regarding several events occurring over days with persistence of symptoms over a period of six months being a prerequisite for definitive diagnosis. The fear may be directed towards various life aspects such as upcoming events, past demeanor and severe scrutiny of one’s ability to perform in competitive situations such as academics. For a definitive diagnosis to be made, at least one physiological manifestation should be evident. Amongst a sample of GAD victims, ninety five percent presented with unwarranted extreme worrying about upcoming events (Stauss, Hersen, Last & Kadzin, 1988). Children with GAD have what scientists have termed a “perfectionist attitude.”
The range of worries includes fear of performance at school, fear of natural calamities, and fear of physical attack amongst others (Silverman & Ollendick, 2005). Characteristically, these children set higher targets even in the absence of duress or concern. In this disorder cognitive disturbances are generalized and not restricted to specific objects or stimulus. The tendency to exaggerate negative outcomes is frequent and they tend to underrate their ability to tolerate non-ideal situations. According to studies, the intensity of symptoms and not the number is the reason for referral of these children for treatment (Weems, Silverman & La Greca, 2000).
The physical components as described in DSM-IV criteria include restlessness, feelings of easy fatigability, disturbed concentration, being irritated easily and sleep disorders. Studies have shown that clinically, more children present with GAD than Specific phobias or SAD with higher incidence in adolescents than in children (Albano, Chorpita, DiBartolo & Barlow, 1995). Related symptoms include concomitant attention deficit and SAD in age range of five to eleven years while depressive tendencies and phobia are common occurrences in adolescents. Further study showed that co-morbid conditions led to more anxiety features without regard to gender and age (Eisen and Engler, 1995).
Panic Disorder
This disorder commonly affects the cognitive aspect of an individual hence it is thought to majorly affect adults. Contrary to past findings, recent documentation has shown that it may also affect youths (Essau, Conradt & Petermann, 1999).The conditions core feature is characterized by sudden panic attacks subsequently followed by persistence of any of the following features for a period of more than four weeks; dreading future attacks or modification of demeanor associated with the attacks.(American Psychiatric Association,1994).This may occur with or without agarophobia.In the presence of agoraphobia, the children dread events or circumstances in which aid cannot be readily accessed. This fear may resemble that of SAD but in panic disorder, the stimulus is the fear of the physical manifestations of the attack or the fear of subsequent attacks while in SAD, anxiety of separation from figures they are attached to.
Diagnosis of this condition in children is difficult since their cognitive aspect is not well developed. In accounted cases non-specific fear of emesis or falling ill has been reported. It is not until early adolescence that autonomic symptoms commence which may encompass fear of increased heartbeat, breathlessness, faintness and loss of self awareness. Attacks are reported to be more prevalent in female subjects than their male counterparts (Hayward et al., 1992).
Medication History
Psychopharmacology entails the utilization of psychoactive drugs in intervention of psychiatric disorders such as anxiety disorders. These agents are involved in neuromodulation of numerous biochemical pathways that regulate the way we react to different situations in life. Many a research, have focused on phenotypic manifestations of anxiety disorders with disregard of what is often termed “silent anxiety disorders”. With this approach, management has mainly been based on intervention of symptoms rather than the underlying factors that lead to anxiety disorders in children. The design of medications is governed by resultant symptoms of the various anxiety disorders such as aggressiveness, unhappiness, hyperactivity and impulsiveness (Gadow, 1992). Furthermore, failure to appreciate the occurrence of co-morbid conditions such as depression and mania greatly affects the choice of medication in management of anxiety disorders.
Untoward effects associated with some medications used in management of anxiety disorders may be overlooked since some of these drugs precipitate anxiety-like conditions. Antidepressants may cause reversible anxiety that occurs within the first few weeks of treatment and this may mislead healthcare providers that the condition is worsening when in real sense, it is not.
Previous Research
Numerous studies have been carried out to ascertain the prognosis of anxiety in cases where intervention is not initiated. Studies have shown that when anxiety disorders are not managed as soon as they develop, they may result in persistent anxiety disorders that stretch into later years of life (Spence, Rapee, McDonald & Ingram, 2001). Previous research has elaborated the complex pathways that bring about such pathological anxiety conditions as a child matures. Separation anxiety disorder has been shown to extend into adulthood in absence of proper intervention. Furthermore, it results in development of co-morbid conditions such as depression with periodic spontaneous waning to the original state (Mackner, Starr & Black, 1997).
Phobic disorders such as social phobia and agoraphobia have been shown to decrease in severity as a child grows even in the absence of any intervention. Research has shown that children have a better prognosis than adults when it comes to phobic disorders. However, it was demonstrated that phobias have a lasting impact on particular populations of children, where it manifests itself even in adulthood (Essau et al., 2000).
Obsessive-compulsive disorder has been shown to be incapacitating if proper therapeutic interventions are not initiated early in life. Research has shown a correlation between Obsessive-compulsive disorder and other psychiatric disorders in both children and adults. Most children diagnosed with OCD tend to have one or more co-morbid conditions. Furthermore, evidence shows absence of complete diminution in children with obsessive compulsive disorders even with cognitive-behavioral and pharmacological interventions (King, Leonard & March, 1998).
Research carried out to ascertain the prognosis of panic disorders show high incidence of episodic attacks that are intermittent. Panic disorders manifest in children and adults in absence of corrective measures. Research carried out has clearly illustrated consequences of anxiety disorders on the child, its family and society as a whole. This prompted research on better methods to deal with these disorders. Controversies on the best method for management of the various anxiety disorders still exist and a wholesome consensus has not been reached, but a variety of interventions have been established to counter these disorders. These studies assess the best age to initiate interventions to achieve maximum benefits to the child. However, some intervention methods have demonstrates beneficial effects time and again when initiated at specific stages of development of the various anxiety disorders.
Marital discord plays a core role in etiology, progression and maintenance of childhood psychopathologies including childhood anxiety disorders. Marital discord brings about distress in the child resulting in chronic anxiety states such as general anxiety disorder. Divorce and divorce proceedings have been shown to impact heavily on young children precipitating separation anxiety. This form of anxiety occurs since children are forced to choose between one of the parents. As a result, the fear of losing a parent may be over expressed in some children resulting in distressful anxiety disorders.
The problem is even more pronounced in families with children with special requirements, since proper care cannot be initiated when parents are always in conflict. Furthermore, children with special requirements may not receive appropriate care in such circumstances when parents are always in discord. Further research has also shown that children born of parents with one or more anxiety disorders have a high likelihood of developing an anxiety disorder at some point in their life (Orvaschel & Weissmann, 1981).
Approaches to Management of Anxiety Disorders
Two main approaches are used in management of anxiety disorders. These approaches are Psychotherapy which entails several mechanismssuch as Behavioral therapy and Cognitive-behavioral therapy and Psychopharmacotherapy which entails use of medicinal agents as interventions of anxiety disorders. Cognitive-behavioral therapy encompasses a variety of approaches in management of anxiety disorders. Examples of such approaches include somatic control, cognitive streamlining, problem elucidation, publicity and reversion prevention. Different anxiety disorders require different approaches in their management. Sometimes all these approaches are employed in tandem for better management of some of the anxiety disorders. Studies have shown achievement of better results when psychotherapy and pharmacotherapy approaches are used simultaneously as intervention methods. Time of initiation of specific therapies plays an important role in the overall effectiveness of the intervention therapy (Foa & Rothbaum, 1998).
Cognitive-behavioral therapy, a form of psychotherapy has been studied in many settings as an intervention of anxiety disorders. This system is based on the finding that in anxiety disorders, a child’s thought process is altered such that it perceives most situations to be of harmful and dangerous hence eliciting evasive behavior. The cognitive-behavior approach aims at restoring normal response to normal situations in a child. CBT in itself encompasses a myriad of techniques to cover most of the disorders. CBT is employed in several disorders most of which share a common etiological pattern and sympomatology. Studies to evaluate effectiveness of Cognitive-behavioral approach in management of General anxiety disorder, separation anxiety disorder and seasonal affective disorder have demonstrated effectiveness of CBT in anxiety disorders in children (Kendall, Ronan & Epp, 1991). Other studies that compared psychotherapy to pharmacotherapy in seasonal affective disorder showed evidence of superiority of Cognitive-behavioral therapy over pharmacotherapy. An example is a study comparing CBT to pharmacotherapy interventions. Patients whom CBT was used showed far much greater improvement than those on medication. A number of Cognitive-behavioral therapy mechanisms have been devised to cater for different anxiety disorders. These methods incorporate use of the internet in interacting with patients. Similarly patients are encouraged to form peer to peer groups that enable them share experiences and ways in which they manage specific anxiety disorders.
Studies have shown that Psychotherapy as a form of intervention for anxiety disorders is not widely used in the normal settings of management of these disorders. Further studies have shown that failure of patients to adhere on CBT schedule has contributed a lot to the ineffectiveness of this method in management of anxiety disorders.From such studies researchers had to rethink further approaches on management of anxiety disorders. In view of this Psychopharmacotherapy as a management option was reconsidered (Taylor & Chang, 2008)
Psychopharmacotherapy
Psychopharmacology entails the utilization of psychoactive drugs in intervention of psychiatric disorders such as anxiety disorders in both children and adults. The use of drugs in various mental illnesses has been a thorn in flesh of many researchers and patients alike. Some believe psychopharmacotherpy is effective while others believe it is not and brings about unnecessary side effects to the recipient. As a result of this, researchers have set out to study the effectiveness of pharmacotherapy intervention in management of anxiety disorders.
Pharmacological agents are entities designed to target specific biochemical pathways that are implicated in precipitation of anxiety disorders in children (Westra & Stewart, 1998).A multitude of studies on numerous pharmacological agents has resulted in isolation of groups of pharmacological agents that have shown efficacy in management, prevention and treatment of anxiety disorders in children.Such agents include The Selective Serotonin Re-uptake inhibitors(SSRIs),Tricyclic antidepressants (TCAs), Monoamine Oxidase inhibitors(MAOs) and Benzodiazepines. Different agents have been suggested as first-line treatment modalities for the various anxiety disorders (Baldwin et al., 2005).
Choice of pharmacotherapy for a particular anxiety disorder depends on several factors. Scientific evidence detailing the efficacy of a particular psychoactive agent for a specific childhood anxiety disorder is a key component in use of psychotherapy. Other factors include set down protocols and the deleterious effects associated with the medication. Of concern to both scientists and patients are the deleterious effects associated with pharmacotherapy. These side effects result in low compliance by patients especially children.
Research has shown that benzodiazepine agents are effective in control of generalized anxiety disorder, panic disorders, and some forms of phobia. Some specific forms of phobia in children have been shown to respond to beta-blocking agents. Agoraphobia and obsessive compulsive disorders are controlled to some extent by the tricyclic antidepressants. Despite this more research in children needs to be carried out to determine the potential of these psychoactive agents as interventions in childhood anxiety disorders (Baldwin et al., 2005).
Management of panic disorders entails use of fast acting benzodiazepines such as alprazolam and a slow acting agent such as a tricyclic antidepressant (TCA) with minimal deleterious effects. Research has demonstrated that this combination is efficacious since benzodiazepines act on the short term to relieve panic disorders but usually there is waning hence the need for a long acting psychoactive agent that eliminates the chances of waning. Of concern is the ability of antidepressants themselves to result into anxiety in the initial stages of treatment. Though there are no studies elaborating the supremacy of one class of medication to another, the frequency of occurrence of deleterious effects has minimized use of some agents. Controlled trials both in children and adults have shown effectiveness of SSRIs in panic disorder and this group is now considered to be first line in management of panic disorder. Agents such Phenelzine are widely used though little evidence is available to prove their effectiveness (Stahl et al., 2003).
Psychopharmacotherapy and cognitive-behavioural interventions are an integral part of management of social anxiety disorders (Social phobias).Though most of these studies have been carried out in adults; the results have been extrapolated in management of this disorder in children. Research on pharmacological intervention in social phobias is limited but evidence of effectiveness of monoamine oxidase inhibitors is available though side effects limit their application. Use of off-label drugs in management of social phobias is a common practice even though no proof exists for their effectiveness in both children and adults (Versiani et al., 1992).
General anxiety disorder, responds to benzodiazepines especially those of the newer generation such as busipirone which has minimal deleterious effects. Further research elucidates the effectiveness of TCAs in a variety of anxiety disorders such as the general anxiety disorder. The Selective serotonin reuptake inhibitors are considered to be first line in pharmacotherapy of GAD. All psychoactive agents in this class have showed greater activity when compared to placebo in human subjects. Further research has shown that utilization of SSRIs eliminates by a defined margin the error of preconception when combined with the cognitive-behavioural approach. Advanced studies of specific SSRIs such as citalopram show that these agents reduce the anxiety response to situations that elicit anxious behaviour (Hoehn-Saric et al, 2004).Herbal remedies have also been shown to relieve GAD. In studies carried out; a unique extract of Ginkgo biloba called EGb 761 reduces symptoms of GAD (Woelk, Arnoldt, Kiesser & Hoerr, 2007).
Before the 60’s it was common knowledge that Obsessive-compulsive disorder was a condition without remedy. But with advanced research pharmacological agents have been identified to reduce the debilitating effects of this condition and as such improve the quality of life. The best intervention for OCD is psychotherapeutic and it entails a mechanism called the “exposure and response prevention”. A large number of studies carried out on pharmacotherapy modalities of OCD have consistently identified SSRIs to be very effective in control of this anxiety disorder (Stahl et al., 2003).These agents also prevent waning of the condition in adulthood. In contrast, some of the research has implicated pharmacological agents in worsening of the pre existing anxiety disorders or precipitating development of novel mental disorders hence worsening the quality of life child. Despite this, research has shown supremacy of pharmacotherapy in management of General anxiety disorder.
Reason for Research
The research of Psychopharmacotherapy as a modality of intervention in children is an essential undertaking for better management of anxiety disorders. As children grow and develop, these disorders may or may not manifest themselves hence the need to have adequate up to date scientific evidence on proper modalities to successfully manage anxiety disorders whether they occur singly or in conjunction with other conditions.
In majority of studies carried out, adults have been the main subjects under study and results obtained are extrapolated in the management of disorders in children. With this in mind, a research that entails use of psychoactive agents in children is of utmost importance for proper and precise management of anxiety disorders in children.
In management of some medical disorders, children are sometimes assumed to be “small adults”, an approach that can be of harm to them especially in determining the correct dosing regimen of medication. Since most psychoactive agents have a narrow therapeutic window, such an assumption would be suicidal in management of anxiety disorders in children.
. The absence of advanced cognitive and communicative skills in children especially infants makes it difficult to employ psychotherapy intervention in management of anxiety disorders in children hence the need to use novel approaches such as Psychotherapy in such situations for better quality life for the affected child.
Furthermore, advances in molecular cell biology and genetics have led to a deeper understanding of biochemical pathways implicated in various anxiety disorders. Armed with this knowledge, research on proper intervention of these pathways at an early age is of importance. With proper research psychoactive agents targeting defects in the biochemical pathways can be developed to arrest anxiety disorders in children.
References
Abramowitz, J.S. (1997). Effectiveness of psychological and pharmacological treatments for obsessive-compulsive disorder: A quantitative review. Journal of Consulting and Clinical Psychology,65,44-52.
Albano, A.M., Chorpita, B.F., DiBartolo, P. & Barlow D.H. (1995). Comorbidity of DSM-III-R in children and adolescents. New York, NY: Prentice Hall.
Baldwin, D., Anderson, I., Nutt, D.J., Bandelow, B., Bon, A., Davidson, J.R., et al. (2005). Evidence-based guidelines for the pharmacological treatment of anxiety disorders: recommendations from the British Association for Psychopharmacology. Journal of Psychopharmacology, 19:567-596.
Barlow, D. H. (2000). Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. American Psychologist, 55(11), 1245-1263.
Beidel, D.C., Turner, S.M. & Morris, T.L. (2000). Behavioral treatment of childhood social phobia. Journal of Consulting Clinical Psychology, 68, 1072-1080.
Bell-Dolan, D., Last, G. & Strauss, C. (1990). Symptoms of anxiety disorders in normal children. Journal of the American academy of child and adolescent psychiatry, 29,759-765.
Bell-Dollan, D. & Brazeal, T, J. (1993) Separation anxiety disorder, overanxious disorder and school refusal. Child and adolescent psychiatric clinics of north America, 2,563-580.
Bowen, R.C, Offord, D.R. & Boyle, M.H. (1990).The prevalence of over anxious disorder and separation disorder in the community. Journal of the American Academy Of Child and Adolescent Psychiatry, 29, 753-758.
Briggs-Gowan, M., Owens, P., Schwab-Stone, M., Leventhal, J., Leaf, P. & Horwitz, S. (2003). Persistence of psychiatric disorders in pediatric settings. J Am Acad Child Adolesc Psychiatry, 42(11),1360-9.
Carrión, V. G., Weems, C. F., & Reiss, A. L. (2007). Stressing about posttraumatic stress disorder: In reply. Pediatrics, 120, 234-235.
Cobham, V.E., Dadds, M.R. & Spence, S.H. (1997).The role of parental anxiety in the treatment childhood anxiety Journal of consulting clinical psychology, 65,627-635.
Costello, E., Egger, H.L. & Angold, A. (2005). The developmental approach of anxiety disorders: Phenomenology, prevalence and comobidity. Child Adolescent Psychiatry Clinical N Am, 14,631-648.
Eisen, A.R. & Engler, L.B. (1995).Clinical handbook of anxiety disorders in children and adolescents. New York, NY: Prentice Hall.
Esau, C., Conradt, J. & Petermann, F. (2000). Frequency, comorbidity and psychosocial impairment of specific phobias in adolescents. Journal of Clinical Child Psychology, 29, 221-231.
Essau, C.A., Conradt, J. & Petermann, F. (1999). Frequencies of panic attacks and panic disorders in adolescents. Journal of Clinical Child Psychology, 9, 19-26.
Foa, F.B. & Rothbaum, B.O. (1998).Cognitive behavioral therapy. New York, NY Guilford Press.
Fontenelle, L.F., Medlowicz, M. V. & Versiani, M. (2006).Pharmacological treatment of social phobia: Traditional MAOIs and moclobemide. Journal of European Neuropsychopharmacology, 23, 124-128.
Freeman, J., Garcia, A.M., Coyne, L., Leonard, H.L & Compton, S. (2007) Family- based cognitive-behavioral treatment for early childhood OCD: Preliminary findings. American Psychiatric Association, 67, 1-8.
Gadow, K.D.(1992). Paediatric psychopharmacotherapy: A review of recent research. Journal of Child Psychology and Paediatric Psychiatry, 33, 153-190.
Geller, D. A., Bierderman, J., Faraone, S., Bellordre, C., Kim, G., Hagermoser, L., et al. (2001). Disentangling chronological age from age of onset of in children and adolescents with obsessive-compulsive disorder. International Journal of Neuropsychopharmacology, 4,169-178.
Hayward, C., Killen, J., Hammer L., Litt, I.F., Wilson, D.M., Simmonds, C., et al. (1992). Pubertal stage and panic history in sixth and seventh grade girls. American Journal of Psychiatry, 149, 1239-1243.
Hirshfeld,D.R.,Rosenbaum,J.Bierderman,J.,Boldue,E.A,Faraoene,S.V,Snidman,N., et al. (1992). Stable behavioral inhibition and its association with anxiety disorders. Journal of American academy of child and adolescent psychology, 31,103-11.
Kearney, C. A., & Albano, A.M. (2007). When children refuse school: A cognitive behavioral therapy approach. Parent workbook. London: Oxford University Press.
Kendall, P.C., Hedtke, K. & Aschenbrand, S.G. (2006). Behavioral and emotional disorders in adolescents: Nature, assessment and treatment. New York, NY: Guilford Press.
Kendall, P.C., Ronan, K.R. & Epp, J. (1991) Aggression in children-adolescents: A cognitive-behavioral perspectives. Journal of Clinical Childhood Psychology 29,120-124.
Kendler, K. S., Neale, M. C., Kessler, R. C., Heath, A. C. & Eaves, L. J. (1993). A longitudinal twin study of personality and major depression in women. Archives of General Psychiatry, 50, 853-86.
King, R., Leonard, H. & March, J. (1998). Practice parameters in the assessment and treatment of obsessive-compulsive disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 37(5), 27-30.
Krohne, H.W. & Hock, M. (1991). Relationships between restrictive mother-child interactions and anxiety of the child. Anxiety Research Journal, 4,109- 124.
Last, C.G. (1993). Relationship between familial and childhood anxiety disorder anxiety across a lifespan: A developmental perspective. American Psychologist, 12, 94-112.
Leonard, H.L. & Rapoport, J. (1991). Obsessive-compulsive disorder: A textbook of child and adolescent psychology. Washington, DC: American Psychiatric Press.
Livingston, R., Taylor, J.L. & Crawford, S.L. (1988) A study of somatic complaints and psychiatric diagnosis in children. Journal of the American Academy of Child and Adolescent Psychiatry, 27,185-187.
Mackner, L.M., Starr, R. & Black, M. (1997). The cumulative effect of neglect and failure to thrive on cognitive functioning. Child Abuse & Neglect, 21, 691-697.
Morris, T. & March, J. (2004). Anxiety disorders in children and adolescents. New York, NY: Prentice Hall.
Orvaschel, H. & Weissman, M. (1981). Assessing psychopathology in children of psychiatrically disturbed parents. Journal of the American Academy of Child Psychiatry, 20,112-119.
Pine D., Helfinstein, S., Bar-Haim, Y., Nelson, E. & Fox, N. A. (2009).Challenges in developing novel treatments for childhood disorders: Lessons from research on anxiety. Neuropsychopharmacology, 34(1), 213-28.
Schniering, C.A., Hudson J. & Rapee, R.M. (2000). Issues in the diagnosis and assessment of anxiety disorders in children and adolescents. Clinical Psychology Review Journal, 20(4), 453-78.
Silverman, W.K. & Albano, A.M. (1996). The Anxiety Disorders Interview Schedule for DSM-IV-Child and Parent Versions. London: Oxford University Press.
Silverman, W.K. & Ollendick, T.H (2005) Evidence based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34,380-411.
Spence, S., Rapee, R., McDonald, C. & Ingram, M.(2001). The structure of anxiety symptoms among pre-scholars. Behavior, Research and Therapy Journal, 39, 1293-1300.
Staub, E., Tursky, B. & Schwartz G. (1971). Self-control and predictability: Their effects on reactions to aversive stimulation. Journal of Personality and Social Psychology, 71(18), 157-162.
Stauss, C., Hersen, C., Last, M. & Kadzin, A.E. (1988). Association between anxiety and depression in children and adolescents with anxiety disorders. Journal of Abnormal Child Psychology, 16, 57-68.
Steinhause, H., Metzke, C., Meier, M. & Kannenberg, R. (1998). Prevalence of child and adolescent psychiatric disorders: The Zurich epidemiological study. Acta Psychiatry Scand, 98,262-71.
Swedo, S., Rapport, J., Leonard, H.L., Lenane, M. & Cheslow, D.S. (1989). The Mauritius child heath project. International Journal of Epidemiology, 23, 1-24.
Taylor, C.B. & Chang, V. (2008). Issues in the dissemination of cognitive-behavior therapy. Nord Journal Psychiatry, 62(47), 37-44.
Thomas, F., John, D., Richard, D., Timothy, F., Christopher L., Shou-Hua, L., et al. (2006). Bupropion reduces methamphetamine-induced subjective effects and cue-induced craving journal of neuropsychopharmacology. Neuropsychopharmacology Journal, 31, 1537-1544.
Velting, O.N., & Albano, A.M. (2001). Current trends in the understanding and treatment of social phobia in youth. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 42, 127-140.
Weems, C., Silverman, W.K. & La Greca, A.M. (2000).What do youth referred for anxiety problems worry about? Worry and its relation to anxiety and anxiety disorders in children and adolescents. Journal of Abnormal Child Psychology, 28, 63-72.
Westra, H.A. & Stewart, S.H. (1998). Cognitive behavioral therapy and pharmacotherapy: Complementary or contradictory approaches to the treatment of anxiety. Clinical Psychology Review, 18(3), 307-340.
Woelk, H., Arnoldt, K. H., Kieser, M. & Hoerr, R. Anxiety: Prevention and complementary therapies for children and Adolescents. Journal of Holistic and Integrative Medicine, 19, 143-145.