Abstract
The purpose of this theoretical framework is to indicate concepts, theories, and models which guide the realization of the capstone project on the topic of improving hemodialysis treatment adherence by removing barriers and providing patient education. The concepts important for the project include treatment adherence, treatment non-adherence, barriers, patient education, self-care, and self-care agency. The theory selected to support the project is Dorothea Orem’s Self-Care Deficit Nursing Theory. The reason is the theory’s focus on patients’ attitudes and intentions regarding self-care, as well as on approaches to addressing self-care demands. Specific assumptions and variables related to the project are also identified.
Theoretical Framework
Chronic severe diseases, including kidney failure, make patients experience a constant stress. The goal of nurses in this case is to help patients adapt to treatment regimens and to guarantee treatment adherence while addressing a range of barriers and the lack of education regarding hemodialysis (Nobahar & Tamadon, 2016). In the United States, the prevalence of chronic renal failure constantly grows, and the number of patients who need hemodialysis “increased from 340,000 in 1998 to 651,000 in 2010” (Zolfaghari, Sookhak, Kashfi, Sekhavati, & Tabrizi, 2017, p. 1). These patients need to follow specific treatment regimens and participate in regular hemodialysis sessions. To improve their state, patients with kidney failure should follow diets, change their lifestyles, and conduct hemodialysis procedures regularly (Chan, Thadhani, & Maddux, 2014).
However, the problem is that many patients tend to ignore their treatment regimens because of some barriers and problems with treatment adherence. Researchers identified such main barriers to adhering to the regimen and proposed treatment as the lack of knowledge, understanding, and education; safety concerns; the lack of control; and the lack of motivation associated with forgetfulness (Chan et al., 2014; Nobahar & Tamadon, 2016). Thus, although these patients need to follow their treatment plans strictly because of threats to their life, “more than 50% of hemodialysis patients do not adhere to their treatment regimen” (Zolfaghari et al., 2017, p. 1). From this point, the improvement of hemodialysis treatment adherence for patients with chronic renal failure is important to increase the quality of nursing services, as well as the quality of patients’ lives. The focus should be on removing barriers to treatment adherence and improving patient education. Dorothea Orem’s Self-Care Deficit Nursing Theory is selected to provide a theoretical framework for this capstone project because of its orientation to patients’ responsibility for their health and care.
Related Concepts and Definitions
Key concepts which are associated with the development of this project are treatment adherence, treatment non-adherence, barriers, patient education, self-care, and self-care agency. In this section, it is important to discuss these concepts and provide their definitions. Treatment adherence is the key concept identified for this capstone project, and it means following the prescribed treatment plan in an efficient manner and without exceptions in order to guarantee the improvement of a physical state (Chan et al., 2014). On the contrary, treatment non-adherence is a process of ignoring healthcare providers’ prescriptions while causing harm to one’s health and increasing readmissions to hospitals among other negative consequences (Chan et al., 2014). In this project, treatment non-adherence means ignoring the regimen proposed for hemodialysis patients, which can lead to significant negative effects on their health and quality of life.
Barriers are any obstacles which prevent individuals from completing their goals and following their plans. In this project, barriers include factors which prevent patients with renal disease from adhering to their treatment plans. These factors can be both external (costs, the lack of provided education) and internal (the lack of motivation, fears) (Nobahar & Tamadon, 2016). Patient education is another important concept which can be defined as the provision of knowledge regarding a patient’s condition and ways of addressing a health problem with the focus on medication and non-medication treatment. For this project, patient education includes information provided by healthcare professionals regarding the importance of hemodialysis, principles of following a regimen, and principles of changing a lifestyle (Zolfaghari et al., 2017).
Self-care is another concept which means the practice when persons take responsibility for their care and recovery and participate in activities to maintain their health (O’Shaughnessy, 2014). In this capstone project, self-care means hemodialysis patients’ initiatives regarding their care which are reflected in their treatment adherence. One more important concept is the self-care agency which means an individual’s ability to become engaged in care activities. For this project, the focus of these activities is on patients’ responsibility and treatment adherence.
The Theory Guiding the Project
The specific theory which guides this capstone project is Dorothea Orem’s Self-Care Deficit Nursing Theory. It was developed in the 1960s-1980s. The theory represents a combination of such models as “the theory of self-care,” “the theory of self-care deficit,” as well as “the theory of nursing systems” (Queirós, Vidinha, & Almeida, 2014, p. 159). Self-care, as the main idea of the first theory, is a practice of performing certain activities which help patients maintain health. According to Orem’s theory, such care should be intentional and controlled to produce positive effects. In addition to the idea of self-care, Orem also paid much attention to developing such concepts as self-care requisites which can be universal (applied to all individuals) and developmental (reflecting differences in individuals’ development) (Rostami, Badr, & Falah, 2015). These concepts support Orem’s theory of self-care.
As the part of the theory of self-care deficit, it is possible to determine such major ideas as the necessity of a nurse’s care when individuals are limited in opportunities to care for themselves. Another component of the theory is a focus on nursing compensatory and supportive systems, in the context of which nurses can provide care for those patients who cannot focus on self-care (Queirós et al., 2014). The key principles of this theory are the following ones: patients are interested in becoming healthy and focusing on their care; needs of individuals are different; self-care should address universal and developmental needs; individuals should receive some knowledge and education to demonstrate self-care behaviors (Rostami et al., 2015).
Relationship of the Concepts and Theory to the Project
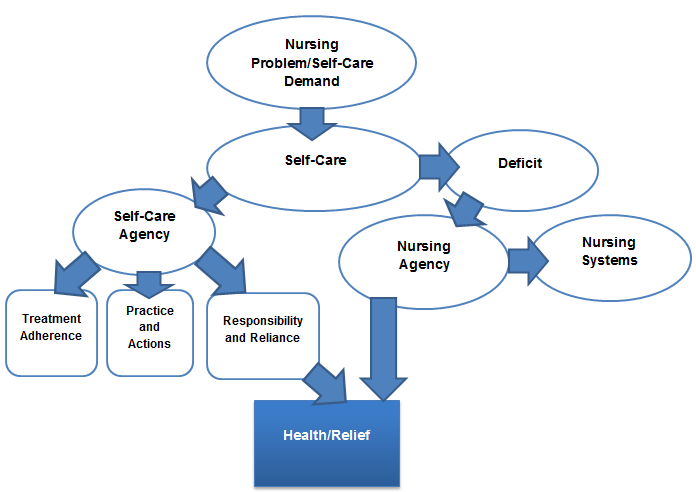
Orem’s Self-Care Deficit Nursing Theory is appropriate to be applied to this project and demonstrate the importance of self-care for those patients who need hemodialysis. Thus, the conceptual model of the project includes such factors as the nursing problem or a self-care demand (chronic renal failure in this case), self-care agency (treatment adherence and activities to improve a health state), nursing agency (nurses’ support based on nursing systems) (O’Shaughnessy, 2014; Queirós et al., 2014). All these factors lead to improving health or, in the context of this project, to receiving some relief. Thus, Orem’s theory accentuates the role of a patient to maintain health and the role of a nurse when there is a self-care deficit. The purpose of this project is to demonstrate how it is possible to improve treatment adherence for hemodialysis patients with the focus on removing barriers and providing education. The model presented in Figure 1 and based on Orem’s Self-Care Deficit Nursing Theory shows that, when patients do not understand the role of self-care, their independence in taking decisions and following treatments should be accentuated. Furthermore, nurses should mobilize their resources, address patient barriers, and provide the required education and support (Queirós et al., 2014).
Assumptions
The following assumptions are proposed for the project:
- The implementation of Orem’s Self-Care Deficit Nursing Theory will improve treatment adherence in hemodialysis patients.
- Improvements in treatment adherence in patients will become a result of explaining the self-care concept and removing barriers to treatment, including fears, the lack of knowledge, safety concerns, the lack of control, and the lack of motivation.
- Improvements in treatment adherence in hemodialysis patients will become a result of providing education and support for patients.
- Those patients who demonstrate treatment non-adherence or a self-care deficit will be ready to understand the principles of the self-care agency.
- Nurses will be ready to support those hemodialysis patients who need assistance in care.
Variables
Variables which should be taken into consideration in this project include nurses’ professional standards and training for nurses. The principles of communication between nurses as healthcare providers and patients are described in professional standards, and it is expected that nurses will pay much attention to educating patients regarding the importance of hemodialysis treatment adherence and possible barriers that they can face (Queirós et al., 2014; Rostami et al., 2015). However, the problem is that nurses can require additional training in order to make patients become aware of psychological, social, and economic barriers to their treatment and motivate them to focus on self-care or receive the professional care.
Conclusion
The theoretical framework based on Dorothea Orem’s Self-Care Deficit Nursing Theory will demonstrate what strategies can be taken in order to improve treatment adherence in hemodialysis patients when they face certain barriers and require additional education. The model accentuates the importance of self-care and the possibility of nurses’ assistance if there is a self-care deficit. The theoretical framework explains that the use of approaches to removing barriers for patients and improving their education regarding hemodialysis treatment can potentially encourage them to become more responsible for their care and avoid ignoring treatment recommendations. It will be possible to reduce complications and improve these patients’ life quality.
Summary
Chronic renal failure is a condition which results in the necessity of regular hemodialysis procedures. Patients with this diagnosis need to adhere to their treatment plans strictly. Nevertheless, there are cases when individuals demonstrate treatment non-adherence because of such barriers as the lack of knowledge, the lack of education, the lack of control, fears, and costs. The project oriented to improving treatment adherence in hemodialysis patients should be based on such theory as Orem’s Self-Care Deficit Nursing Theory because it involves the concepts of self-care and a self-care deficit. While applying this model, it is possible to expect that persons will concentrate on self-care and receive education to improve their health state. Therefore, Orem’s Self-Care Deficit Nursing Theory can be discussed as an appropriate model to guide this capstone project.
References
Chan, K. E., Thadhani, R. I., & Maddux, F. W. (2014). Adherence barriers to chronic dialysis in the United States. Journal of the American Society of Nephrology, 25(11), 2642-2648.
Nobahar, M., & Tamadon, M. R. (2016). Barriers to and facilitators of care for hemodialysis patients: A qualitative study. Journal of Renal Injury Prevention, 5(1), 39-44.
O’Shaughnessy, M. (2014). Application of Dorothea Orem’s theory of self-care to the elderly patient on peritoneal dialysis. Nephrology Nursing Journal, 41(5), 495-497.
Queirós, P. J., Vidinha, T. S., & Almeida, A. J. (2014). Self-care: Orem’s theoretical contribution to the nursing discipline and profession. Revista de Enfermagem, 4(3), 157-163.
Rostami, F., Badr, F. R., & Falah, N. (2015). A survey of the impact of using Orem self-care model on adequacy of dialysis in hemodialysis patients. Bulletin of Environment, Pharmacology and Life Sciences, 4(5), 19-23.
Zolfaghari, M., Sookhak, F., Kashfi, S. H., Sekhavati, E., & Tabrizi, R. (2017). The effects of cognitive behavioral interventions on removing barriers to treatment adherence in hemodialysis patients. Asian Journal of Pharmaceutical and Clinical Research, 10(1), 1-5.